What’s a ‘FODMAP’?
FODMAP is an acronym for a group of short-chain carbohydrates (sugars):
- Fermentable Oligosaccharides (e.g. fructans and galacto-oligosaccharides)
- Disaccharides (e.g. lactose)
- Monosaccharides (e.g. excess fructose) and
- Polyols (e.g. sorbitol, mannitol, maltitol, xylitol and isomalt)
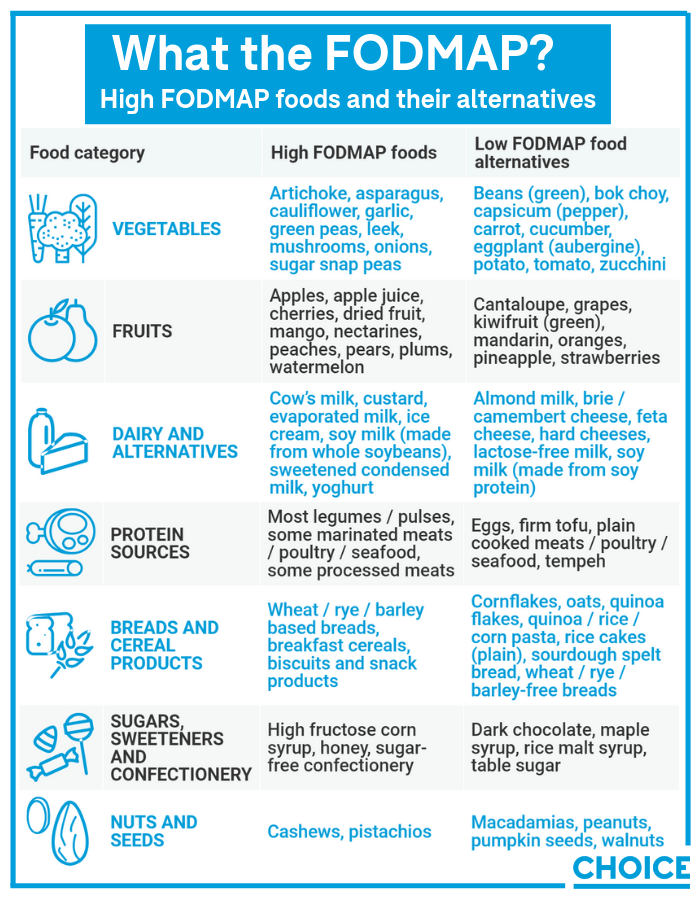
These sugars are fermented by the bacteria that live inside our intestines and are present in many of the foods we eat. Common high-FODMAP foods include garlic, onions, apples, milk, mushrooms, bread and chickpeas, among many others.
For 85% of the population, the fermentation of these sugars isn’t an issue, but for one in seven people, some high-FODMAP foods can trigger the uncomfortable and potentially debilitating symptoms of irritable bowel syndrome (IBS). For these people, the low-FODMAP diet can be life-changing.
Who should try a low-FODMAP diet?
The low-FODMAP diet isn’t for everybody; you won’t lose weight on it, burn tummy fat or improve your general health.
In fact, without an IBS diagnosis from a doctor or dietitian, embarking on this highly restrictive diet has the real potential to cause unnecessary damage to the health of your gut microbiome.
But, if you do have IBS, the short-term Monash University Low-FODMAP diet™ is a diagnostic tool that can help you identify your trigger foods, and reduce and manage your IBS symptoms in the long term.
Can it cure people of IBS?
No, but it can help you manage symptoms.
There’s no known cure for IBS. It’s a chronic condition that needs to be managed long term, which is where the low-FODMAP diet comes in.
Recent studies have revealed the low-FODMAP diet reduces IBS symptoms for around 86% of people. In addition, symptoms can continue to improve with the reduction of triggering high-FODMAP foods for a long time, provided these foods are avoided or significantly limited.
For people with IBS, the low-FODMAP diet can be life-changing
“The idea is to settle the symptoms right down,” says Nicole Dynan, accredited practising dietitian and spokesperson for the Dietitians Association of Australia (DAA).
“So, it might just be that you’ve been overloading yourself with that particular sugar group, and if we find your personal tolerance level then there’s no reason you can’t go on tolerating an amount of that particular group.”
What is a low-FODMAP diet?
Monash University’s Department of Gastroenterology launched a major study in 2005 to see if IBS could be managed through diet, and found four classes of short-chain carbohydrates (sugars) that were poorly absorbed in the small intestine.
These sugars attract water into the bowel, and when they reach the large intestine they’re fermented by the resident gut bacteria and, in combination with a sensitive gut, can result in IBS symptoms such as bloating, distension, pain, constipation and diarrhoea.
It isn’t just another fad diet
Over the years the Monash University research team has shown in numerous studies that a diet low in high-FODMAP foods can help ease the symptoms of IBS.
Subsequently, the team developed the Monash University Low-FODMAP diet™, now considered frontline therapy for IBS around the world.
How does it work?
The first thing you should know about the low-FODMAP diet, says Associate Professor Jane Muir, Head of Translational Nutrition Science in the Department of Gastroenterology at Monash University, is that it isn’t just another fad diet.
“It is important to emphasise here that the low-FODMAP diet is a diet therapy for a medically diagnosed condition – IBS,” she says.
Muir describes the FODMAP diet as three-phased.
Step one: “Patients swap high-FODMAP foods for low-FODMAP alternatives, thus lowering their overall FODMAP intake, which they follow for around two to six weeks,” she explains.
“If they notice an improvement in their IBS symptoms in step one, they progress to step two.”
Step two: This should take between eight and 12 weeks and involves introducing high-FODMAP foods back into the diet, one at a time, and increasing the amount each day to determine which foods trigger IBS symptoms, and how much can be tolerated.
Step three: A ‘personalised’ low-FODMAP plan for the future is devised, which is minimally restrictive and intended to maintain an adequate level of symptom control.
“Well-tolerated foods and FODMAPs are included in the personalised FODMAP diet, while poorly tolerated FODMAPs are restricted, but only to a level that is necessary to maintain adequate symptom control,” says Muir.
For short-term use only
The low-FODMAP diet is a diagnostic tool and isn’t recommended for long-term use.
“The effect of FODMAP restriction on the gut microbiota occurs because some FODMAPs (e.g. fructans and galacto-oligosaccharides) are a fuel source for good bacteria in our gut; that is, they’re ‘prebiotics’,” says Dr Jane Varney, research dietitian with the Department of Gastroenterology at Monash University.
“If poorly implemented, the diet can also restrict intake of some nutrients, such as calcium and fibre. This is one reason why we strongly recommend people only implement the diet short term – and under the guidance of a FODMAP-trained dietitian.”
How to start a low-FODMAP diet
The first thing you should do, if you haven’t already been diagnosed with IBS, is to go to your local GP and have tests done to rule out other medical conditions that present a range of similar symptoms, such as coeliac disease, gluten sensitivity, anxiety, depression and stomach or colon cancer.
Then, get a referral from your GP to a DAA-qualified dietitian who has expertise in food intolerances and the low-FODMAP diet.
“Go to the DAA website and search for an Accredited Practising Dietitian in your area,” Dynan says.
Under the supervision of your dietitian, you’ll embark on stage one of the low-FODMAP diet and remove all high-FODMAP foods from your diet for a specified length of time.
Some of the more common high-FODMAP foods, along with their low-FODMAP alternatives, are as follows:
Dynan says she provides any IBS patients embarking on the low-FODMAP diet with resources from the Gastroenterological Society of Australia (GESA).
“We look through lists of common foods they might be eating that are in the high-FODMAP lists and we highlight them,” she says.
“Then I show them a sample diet and what they’re able to actually eat in that first phase, swapping high-FODMAP foods for low-FODMAP foods.”
To ensure her patients maintain good nutritional balance throughout the process, she also recommends they download the Monash University low-FODMAP diet app (iOS, $12.99/Android, $9.50).
“It’s a traffic-light system for high- and low-FODMAP foods and it guides them so they’re able to implement the diet really effectively. The app also has recipes on there and things like that … it’s a great resource,” says Dynan
People may experience almost immediate relief from IBS symptoms during the initial phase of the diet, however, it’s important for gut health not to remain in this phase for an extended period of time.
Once high-FODMAP foods are recognised as the culprits, moving into the reintroduction phase works to determine which high-FODMAP foods trigger IBS symptoms, and how much of these foods the body can tolerate.
Medicare subsidies
Medicare provides Chronic Disease Management Plans for people with long-term chronic health conditions, which subsidises appointments with allied healthcare professionals – in this instance, a dietitian.
“It’s up to your GP to determine if your condition qualifies,” says Dynan. “If it does, for each of the subsidised consultations via Medicare you get a $52.95 rebate off the cost.”
CASE STUDY: “Within a couple of days, I felt normal for the first time in years”
CASE STUDY: “I noticed improvements to my symptoms within days”
Can I DIY the FODMAP diet?
It’s not advised. IBS symptoms mimic those of many other gastrointestinal disorders, such as coeliac disease, inflammatory bowel disease and bowel cancer, so it’s important that these are ruled out and an IBS diagnosis is made by a medical doctor before embarking on the FODMAP diet, explains Muir.
“Individuals who are experiencing gastrointestinal symptoms should consult their doctor, and once the diagnosis of IBS is made, the doctor can refer them to a qualified dietitian to explore the use of diet therapy to control the symptoms,” she says.
We strongly recommend people only implement the diet short term – and under the guidance of a FODMAP-trained dietitian
The low-FODMAP diet is a highly restrictive diet that, without the supervision of a dietitian, may result in inadequate fibre, calcium and other essential nutrients. A dietitian ensures the diet is implemented properly to achieve the best diagnostic results, and that nutrient requirements are met.
The role of the dietitian
Dynan says a dietitian plays an essential role in the low-FODMAP diet.
“I had one chap come in, in his 40s. He’d been to every doctor, every specialist, had every scan, every test, every scope possible because he’d had chronic diarrhoea for two years and he couldn’t get resolution on it,” she says.
“[After doing the low-FODMAP diet] it came down to onion for him and he came back two weeks later and said to me, ‘I can’t believe I went to professors, all the gurus, and it’s the little dietitian who solved my problem’.”
The food industry is taking note
As more people learn about the impressive success for IBS sufferers on the low-FODMAP diet, canny food manufacturers are producing food products to cater to the growing number of FODMAP adherents. But are they worth the added cost?
“When I first started seeing FODMAP products on the supermarket shelves twelve or so months ago, I was actually quite shocked,” says Dynan.
“It’s a medical diet, not something that the public should really be embarking on on their own.
“Also, these products aren’t necessarily healthier. As with anything processed … you should look carefully at the nutrition label for things like salt, saturated fat and sugar content.”
Increased convenience
That said, these readily accessible products do offer increased convenience for consumers on a low-FODMAP diet.
“We’re all very time poor so it does give people who are on the diet easy choice, and there’s obviously a demand for them,” says Dynan.
[FODMAP products] aren’t necessarily healthier … you should look carefully at the nutrition label for things like salt, saturated fat and sugar content
Monash University’s food certification program stamps a wide range of foods in Australian supermarkets suitable for those following step one and step two of the low-FODMAP diet.
“All products included in the Monash University Low-FODMAP CertifiedTM program have been laboratory tested by the independent team at Monash University, using validated scientific methods to ensure they meet the low-FODMAP criteria,” Varney says.
FODMAP Friendly is another low-FODMAP certification stamp, which claims to be the “only registered certification trademark worldwide certifying FODMAP levels in food products that have been laboratory tested to be low in FODMAPs” and designed to enable people with IBS to “shop and eat with confidence”.
Increased cost
But these low-FODMAP certified products do come at a significantly increased cost compared with foods that are naturally low FODMAP. Varney says there are a number of reasons why this may be the case.
“Specialty products often include ingredients that are more expensive, production volumes may be lower (meaning there are more overheads to cover per unit of production) or there may have been significant investment in the development process to ensure that flavours and textures are optimal,” she says.
“There are also costs associated with certifying low-FODMAP products, and food labelling laws in Australia prohibit manufacturers from making claims about FODMAP content without inclusion in a certification program.”
https://www.choice.com.au/health-and-body/conditions/hayfever-and-allergies/articles/what-is-a-low-fodmap-diet?utm_source=facebook&utm_medium=social&fbclid=IwAR3P0cKgHTi8bzS0OaceVLKa34WRVY5JVK1odxu7TLWTyXE3qJ7Ipi0NQAo
 Childhood microbiome health: the secret to resisting illness.👨👩👧👦🤗
Childhood microbiome health: the secret to resisting illness.👨👩👧👦🤗









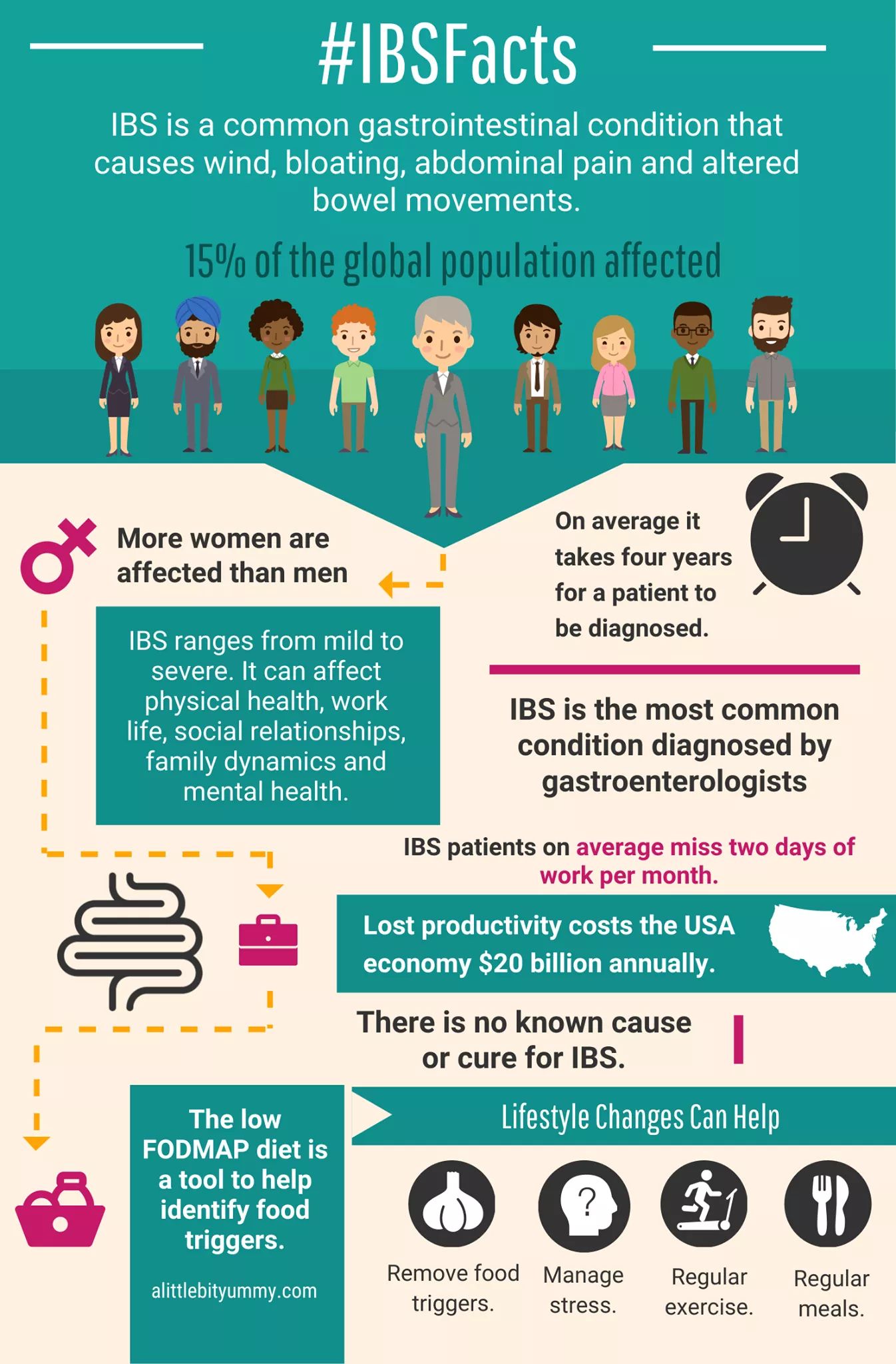 It’s time to spread the word about IBS. IBS has a huge impact on our communities and often carries unnecessary stigma! ❤️
It’s time to spread the word about IBS. IBS has a huge impact on our communities and often carries unnecessary stigma! ❤️