If your busy lifestyle leaving you feeling tired, stressed and out of balance?
Do You Need More Magnesium?
While stress is a key culprit in reducing magnesium, there are other factors which can diminish levels of this vital mineral including reproductive hormonal changes (e.g. pregnancy) and long-term use of the oral contraceptive pill.3
Further, modern food processing techniques can contribute to a reduction of dietary magnesium consumed.4 If you are one of the many women with hormonal complaints such as premenstrual syndrome (PMS),5 menstrual migraine,6 polycystic ovarian syndrome (PCOS)7 and symptomatic menopause;8,9 your magnesium levels may be 20-30% lower than those who are symptom free.
For more on hormonal conditions read this article.
That’s not all though. Many women turn to coffee and/or alcohol as a way of raising energy or ‘winding down’; however, research shows an excess intake of these can also deplete magnesium levels.10 If this is you, it may well be time to explore some new invigorating or stress management strategies, such as swapping out one of your fitness classes for some restorative yoga, or perhaps a regular walk in nature.
How Stress Wields a Hefty Blow
Even if you don’t feel stressed, the persistent busyness of everyday life is still seen as a type of stress which can take its toll on your body. The ‘stress response’ causes the adrenal glands to release hormones (e.g. cortisol) and neurotransmitters (messenger molecules such as adrenaline, noradrenaline, and a small amount of dopamine). However, this leads to magnesium being released from your cells, and excreted via the urine, lowering levels and amplifying the stress response.11 Essentially, whilst you have an increased demand for magnesium when you are stressed, your body offloads it when you need it most! This vicious cycle can leave you low in magnesium, with flow-on effects on healthy nervous system function and hormonal balance.
The Magic of Magnesium for Female Health

Whilst the mechanisms impacting magnesium levels may seem complex (and maybe alarming!), the solution is actually very simple – focus on incorporating foods rich in magnesium into your daily diet (e.g. dark green leafy veg, quinoa, almonds, and black beans are all options); plus you can rapidly replenish your magnesium levels through quality supplementation. This way you can support a healthy stress response, but also help tackle any premenstrual migraines, period pains, and/or mood symptoms (e.g. mood swings, irritability, anxiety).12
Moreover, magnesium supplementation can help manage conditions such as endometriosis and fibroids, by supporting healthy oestrogen metabolism and clearance,13,14,15 therefore helping restore balance.
Interestingly, magnesium also helps to prevent bone loss approaching menopause, by reducing the inflammation and free radical damage that can drive bone deterioration occuring post-menopausally.16 As you can see, virtually all women could benefit from magnesium at some point in their lives.
Which Form of Magnesium is the Best?
This is an understandable question with so many to choose from, and important as not all forms of magnesium are equal. Look for amino acid chelates, such as magnesium bisglycinate (e.g. Meta Mag®). This has a unique biochemical shape that makes it the most effectively absorbed form of magnesium,17,18 which is what you want – magnesium getting to the areas of your body where it is needed most, so you can feel it’s effects.
If you have hormonal symptoms (such as PMS or period pain), magnesium works well alongside:
- Boswellia: a herb with potent anti-inflammatory and analgesic effects19 to reduce PMS symptoms and period pain;
- Chromium: alleviates cravings associated with PMS;20
- Chamomile: helps relieve stress, calms, and supports healthy mood;21 and
- Broccoli: aids in the elimination of hormone-disrupting environmental chemicals.22,23 (This topic was discussed in an earlier blog.)
As navigating hormonal conditions can be tricky – speak to a natural healthcare Practitioner for the most appropriate solution for your needs for best results.
Create a Life of Hormonal Bliss
Stress management is an essential part of enjoying healthy hormonal balance, but there is more you can do. Take a holistic perspective and support your overall health by engaging in regular physical activity, drinking 1-2 litres of water daily, and ensuring your diet is rich in ‘good’ fats such as avocado, oily fish (e.g. salmon, anchovies, mackerel), and nuts and seeds (your body requires good fats to make hormones).
Busy woman have better things to do than spend time curled up in bed with period pain, or inconvenienced by some other hormonal symptom. If this is you, begin today to turn things around by ensuring you have your stress under control, and speaking to your Practitioner about your need for magnesium (or about any other health related questions you may have) so you can continue to take on the world happy and healthy!
References
1. Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. 2011 Jan;15(1):18-22.
2. Eby GA 3rd, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010 Apr;74(4):649-60.
3. Eby GA 3rd, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010 Apr;74(4):649-60.
4. Eby GA 3rd, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010 Apr;74(4):649-60.
5. Abraham GE, Lubran MM. Serum and red cell magnesium levels in patients with PMT. Am J Clin Nutr. 1981;34:2364-6. doi: 10.1093/ajcn/34.11.2364.
6. Mauskop A, Altura BT, Altura BM. Serum ionized magnesium levels and serum ionized calcium/ionized magnesium ratios in women with menstrual migraine. Headache. 2002 Apr;42(4):242-8. PMID: 12010379.
7 Chakraborty P, Ghosh S, Goswami SK, Kabir SN, Chakravarty B, Jana K. Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol Trace Elem Res. 2013 Apr;152(1):9-15. doi: 10.1007/s12011-012-9592-5.
8. López-González B, Molina-López J, Florea DI, Quintero-Osso B, Pérez de la Cruz A, Planells del Pozo EM. Association between magnesium-deficient status and anthropometric and clinical-nutritional parameters in postmenopausal women. Nutr Hosp. 2014 Mar 1;29(n03):658-664. doi: 10.3305/nh.2014.29.3.7198.
9. Okyay E, Ertugrul C, Acar B, Sisman AR, Onvural B, Ozaksoy D. Comparative evaluation of serum levels of main minerals and postmenopausal osteoporosis. Maturitas. 2013 Dec;76(4):320-5. doi: 10.1016/j.maturitas.2013.07.015.
10. Johnson S. The multifaceted and widespread pathology of magnesium deficiency. Med Hypotheses. 2001 Feb;56(2):163-70.
11. Cuciureanu MD, Vink R. Magnesium and stress. In: Vink R, Nechifor M. Magnesium in the central nervous system. Adelaide: University of Adelaide Press; 2011. p. 251-268.
12. Parazzini F, Di Martino M, Pellegrino P. Magnesium in the gynaecological practice: a literature review. Magnes Res. 2017 Feb 1;30(1):1-7. doi: 10.1684/mrh.2017.0419.
13. Brown RC, Bidlack WR. Dietary magnesium depletion: p-nitroanisole metabolism and glucuronidation in rat hepatocytes and hepatic microsomal membranes. Proc Soc Exp Biol Med. 1991 May;197(1):85-90. PMID: 1902295.
14. Maruti SS, Li L, Chang JL, Prunty J, Schwarz Y, Li SS, et al. Dietary and demographic correlates of serum beta-glucuronidase activity. Nutr Cancer. 2010;62(2):208-19. doi: 10.1080/01635580903305375.
15. Balthazart J, Baillien M, Charlier TD, Cornil CA, Ball GF. Multiple mechanisms control brain aromatase activity at the genomic and non-genomic level. J Steroid Biochem Mol Biol. 2003 Sep;86(3-5):367-79. PMID: 14623533.
16. Castiglioni S, Cazzaniga A, Albisetti W, Maier JA. Magnesium and osteoporosis: current state of knowledge and future research directions. Nutrients. 2013 Jul 31;5(8):3022-33. doi: 10.3390/nu5083022.
17 Albion Human Nutrition. Magnesium: Clinical and health benefits still without limits. Albion Research Notes. 2003 Oct;12(3):1-4.
18. Siebrecht S. Magnesium bisglycinate as safe form for mineral supplementation in human nutrition. Int J Orthomol Rel Med. 2013;144:1-16.
19. Sharma A, Bhatia S, Kharya MD, Gajbhiye V, Ganesh N, Namdeo AG, et al. Anti-inflammatory and analgesic activity of different fractions of Boswellia serrata. Int J Phytomed. 2010;2(1). doi: 10.5138/ijpm.2010.0975.0185.02015.
20. Brownley KA, Girdler SS, Stout AL, McLeod MN. Chromium supplementation for menstrual cycle-related mood symptoms. J Diet Suppl. 2013 Dec;10(4):345-56.
21. Amsterdam JD, Li Y, Soeller I, Rockwell K, Mao JJ, Shults J. A randomized, double-blind, placebo-controlled trial of oral Matricaria recutita (chamomile) extract therapy for generalized anxiety disorder. J Clin Psychopharmacol. 2009 Aug;29(4):378-82.
22. Boddupalli S, Mein JR, Lakkanna S, James DR. Induction of phase 2 antioxidant enzymes by broccoli sulphoraphane: perspectives in maintaining the antioxidant activity of vitamins A, C, and E. Front Genet. 2012 Jan 24;3-7. doi: 10.3389/fgene.2012.00007.
23. Riedl MA, Saxon A, Diaz-Sanchez D. Oral sulphoraphane increases Phase II antioxidant enzymes in the human upper airway. Clin Immunol. 2009;130: 244–25. doi: 10.1016/j.clim.2008.10.007.
Do the highs and lows of (PMS), pelvic pain or heavy flow hamper normal functioning around the time of your period?🤪🤯🤦♀️
Oestrogen is predominately thought of as a female hormone; but just as women have small amounts of the male hormone, testosterone – men also need some oestrogen (albeit at lower levels) for optimal health.
Oestrogen wears many hats, and they’re not all related to reproduction!
It also supports brain health. For example, it has been linked to slowing down the ravages of ageing and is protective against many neurological conditions such as Alzheimer’s disease, schizophrenia and depression.1 Oestrogen is also considered the beauty hormone; she plays a role in collagen production and moisture retention for supple skin,2 helping you looking more youthful! She is part of the reason why women retain hair on their heads, but have thinner hair elsewhere on the body. Oestrogen will also help bones remain strong by preventing calcium loss, and even supports healthy cholesterol metabolism (see Figure 1).
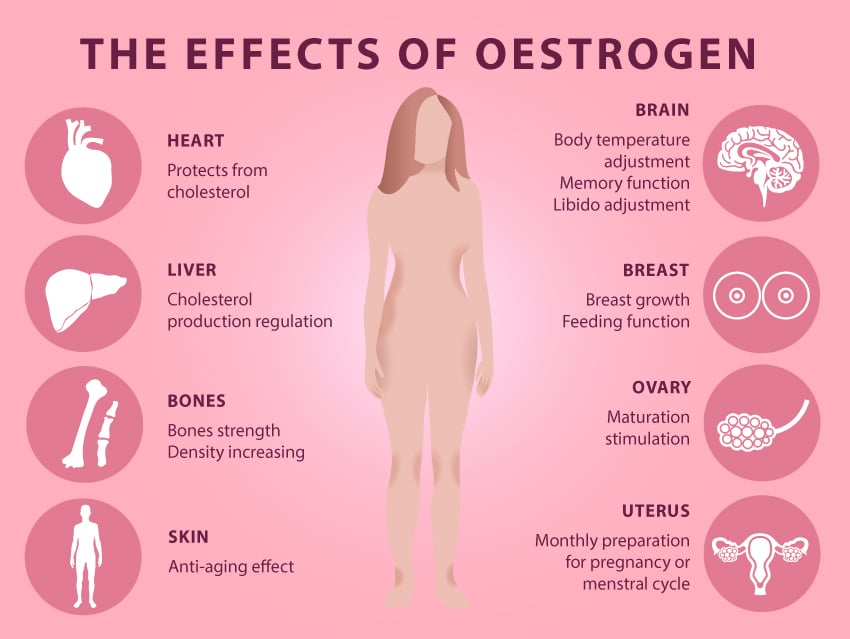
Figure 1: The Many Effects of Oestrogen.
All that said, oestrogen’s primary function is as a reproductive hormone. Levels begins to increase in young girls in puberty, around the time their periods begin. It is produced mainly by the ovaries, and will go on to shape and grow the breasts, the uterus and it’s lining (known as the endometrium) – essentially preparing the female body for reproduction. Interestingly, males also rely on oestrogen for the all-important task of creating healthy sperm!
Fun Fact: Did you know that during pregnancy, oestrogen levels are 1000 times higher than in non-pregnant women? This increase helps to expand the uterus to make space for the developing foetus and prepares the breasts for lactation.3
Intracrinology – Intra What?
I know I mentioned earlier that oestrogen is produced primarily by the ovaries but this sneaky hormone can also be synthesised in other tissues in the body including the breast, the brain and even in body fat! Known as the science of intracrinology, the study of hormone levels in different tissues can give some fascinating insights into the activity of oestrogen throughout the body. As shown in Figure 2 below, many factors (such as increased production in various tissues and impaired detoxification) can disrupt the delicate balance of hormones and in some cases lead to having too much.
Excess oestrogen may result in symptoms such as period pain, heavy flow, PMS and even more serious presentations such as endometriosis,4 fibroids5 and breast cancer.6
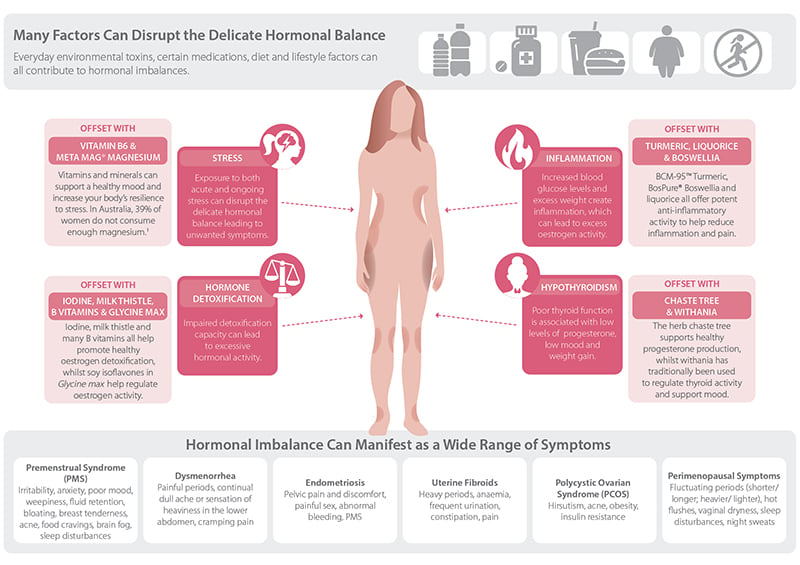
Figure 2: Many Factors Can Disrupt Hormonal Balance, But There Are Things You Can do to Correct This.
To give another example – if a woman is overweight, the extra fatty tissue can hold more oestrogen in the body, which can potentially lead to oestrogen excess and a worsening of hormonal symptoms. Learn about more ways hormones can become disrupted here.
Further, living in the modern world brings a constant exposure to environmental toxins such as plastics and other chemicals; those that have hormonal effects are known as endocrine disrupting chemicals (EDCs). EDCs such as bisphenol A (BPA) found in the lining of tins can actually increase oestrogen and change the way it works in the body. Read more about this here.
Be Proactive About Keeping Oestrogen in Balance
If your pain, PMS or hormonal symptoms may be caused by too much oestrogen, then it’s time to take back control. There are many positive steps you can take towards rebalancing your hormones.
Many herbs and nutrients can be extremely beneficial in reigning in out-of-control hormones. Isoflavones from soy are used to support women’s healthy oestrogen levels by modulating oestrogen receptors (the binding sites on the cells).7 This means that soy can effectively instruct cells to promote the healthy actions of oestrogen and turn down the dial down on the more negative impacts. Read more about soy in this article. Other natural medicines such as magnesium, broccoli, rosemary, and BCM-95™ Turmeric all have positive effects on supporting healthy oestrogen metabolism, helping to restore a state of balance.
There are also some simple strategies you can adopt on a daily basis to place you on the path of healthy oestrogen balance. Follow the healthy hormone dietary and lifestyle tips in Figure 3 below. Other suggestions include not microwaving food in plastic containers, and swapping your plastic drinking bottles for glass or stainless steel – this can help reduce the impact of EDCs exposure. For more simple tips to detox your environment check out this blog.

Figure 3: Healthy Hormone Diet and Lifestyle Tips.
By gradually changing your habits you can reduce exposure to harmful EDCs, improve your oestrogen metabolism, and maintain the beneficial effects that the beautiful hormone called oestrogen may bring. If you would like more support in improving hormonal harmony and freeing yourself from the symptoms of oestrogen imbalance, speak to your local natural healthcare Practitioner today.
References
1. Cutter WJ, Norbury R, Murphy DGM. Oestrogen, brain function, and neuropsychiatric disorders. J Neurol Neurosurg Psychiatry.2003 Jul;74(7):837-840.
2. Shah MG, Maibach HI. Estrogen and skin. An overview. Am J Clin Dermatol. 2001;2(3):143-50. PMID: 11705091
3. Greenspan FS, Gardner DG. Basic and clinical endocrinology. 6th ed. Sydney, Australia: Lange Medical Books/McGraw-Hill; 2001. p. 575-602.
4. Ferrero S, Remorgida V, Maganza C, Venturini PL, Salvatore S, Papaleo E, et al. Aromatase and endometriosis: estrogens play a role. Ann N Y Acad Sci. 2014 May;1317:17-23. doi: 10.1111/nyas.12411
5. Bulun SE, Lin Z, Imir G, Amin S, Demura M, Yilmaz B, et al. Regulation of aromatase expression in estrogen-responsive breast and uterine disease: from bench to treatment. Pharmacol Rev. 2005 Sep;57(3):359-83. doi: 10.1124/pr.57.3.6.
6. Chetrite GS, Cortes-Prieto J, Philippe JC, Wright F, Pasqualini JR. Comparison of estrogen concentrations, estrone sulfatase and aromatase activities in normal, and in cancerous, human breast tissues. J Steroid Biochem Mol Biol. 2000 Jan-Feb;72(1-2):23-7. PMID: 10731634.
7. Kuiper GG, Lemmen JG, Carlsson B, Corton JC, Safe SH, van der Saag PT, et al. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology. 1998 Oct;139(10):4252-4263.
We all have those days…😉
So what is MANOPAUSE?

Testosterone levels begin to rise in puberty, reach their maximum in a man’s early twenties, and gradually begin to decline from then on. From about the age of 30 men tend to lose about 1% of their testosterone each year – this is normal.
However, as average peak testosterone levels in men have dropped by approximately 20% over the past 40 years, more and more men are experiencing the negative effects of lower testosterone as they age.
Everyone has heard of menopause, the stage of life whereby a women’s sex hormone levels begin to decline. The use of the term ‘manopause’ (or andropause) however is becoming increasingly common, used to describe the correlating condition in ageing males. Some cardinal symptoms of ‘manopause’ include:
- A reduction of sexual thoughts or desire;
- Trouble achieving or maintaining an erection;
- Lower energy levels;
- Mood changes;
- Loss of muscle mass and bone density;
- Reduction in cognitive function; and/or
- Mood disturbances.
Under normal circumstances, testosterone production is tightly regulated within the body. Initially, signalling hormones are produced by the brain, and travel to the testicles to stimulate testosterone production. As testosterone production increases, the brain receives the message there is enough testosterone within the body and stops telling the testicles to produce it. Once levels start to fall, the brain then produces more signalling hormones to stimulate the production of testosterone. This feedback system is what keeps levels of testosterone optimal and the male body healthy.

However, there are a number of factors that can interfere with normal testosterone production and utilisation:
- Once produced, testosterone can be converted into other hormones by enzymes, the two most important called aromatase and 5-alpha reductase. Increased activity of these enzymes can contribute to symptoms of ‘manopause’ by reducing levels of available testosterone.
- Aromatase is found particularly in fat tissues, and it’s activity is up-regulated by inflammation. Aromatase actually converts testosterone to oestrogen, meaning excess weight and inflammation can cause a reduction in testosterone and an increase in oestrogen (which we don’t want too much of in men).
- 5-alpha reductase converts testosterone to a very active form of testosterone called dihydrotestosterone (DHT). While DHT promotes growth in skeletal muscle, too much can also cause the prostate to enlarge (a condition known as benign prostate hyperplasia) and trigger hair loss in hereditary male pattern baldness. Unfortunately, this activity of DHT is largely determined by genetics.
- Nutritional deficiencies can also inhibit the production of testosterone.
Adequate intake of protein, essential fatty acids, zinc and selenium is crucial to provide the necessary building blocks for testosterone production.
- Chronic stress can also reduce testosterone production in a number of ways.
- The ‘ingredients’ (or structural components) required for testosterone production are also used to produce the stress hormone cortisol. Excess production of stress hormones on a long-term basis reduces the amount of ingredients available for testosterone production.
- Cortisol levels can also directly inhibit testosterone production in the testes, as well as the production of the testosterone signalling hormones in the brain.

While there may be complex processes reducing testosterone production, the good news is that many of these can be addressed by simple diet and lifestyle interventions:
- Eat a balanced diet rich in antioxidants, minerals and essential fatty acids to provide all of the building blocks for healthy testosterone production.
- Maintain a healthy body composition, keeping body fat levels down to reduce the conversion of testosterone to oestrogen by aromatase.
- Tackle inflammation by addressing lifestyle factors such as sugar and alcohol consumption, further reducing aromatase activity.
- Learn to manage stress effectively, and ensure good quality sleep to regulate cortisol production, which is crucial for maintaining healthy testosterone levels as you age.
Lastly, there are a number of herbs that have been shown to support testosterone levels and male reproductive health. For example, Tribulus terrestris or ‘tribulus’ has been shown to enhance testosterone in animal studies, and has a long history of use in traditional Ayurvedic medicine to support virility and sexual desire. Similarly, the intriguingly named ‘horny goat weed’ (whose correct Latin name is Epimedium sagittatum) is a traditional male tonic indicated for impotence, as an aphrodisiac, and to enhance sperm production. For optimal results, these herbs should be combined with supplementary zinc (if required), along with the diet and lifestyle strategies above.
Even if the more superficial aspects of testosterone deficiency are not of concern, the role that testosterone plays in wellness and ageing means that all men who wish to live a long and healthy life should be looking to support their testosterone levels in a natural, holistic manner. So if you are feeling fatigued or cranky, your mojo isn’t wasn’t it used to be or you notice that you are losing muscle mass, it could mean that you have low testosterone. If so, work with a qualified healthcare Practitioner to uncover and address the underlying causes, such as those discussed above, to ensure your quality of life now and into old age.
We all know that feeling…😍🍃
How can you prepare for the FLU SEASON?🤧
Are your prepared for the cold and flu season? You might be feeling fine right now but even the healthiest of us can succumb to a stray virus at this time of year, resulting in days off work and…even worse…keeping you indoors and missing out on the things you love to do. Fortunately there are some surprisingly helpful little microbes you may not know about that are your winter allies – capable of helping your immune system search out viral invaders and reducing the chance of an infection taking hold. These little microbes are probiotics.
Knowing the Strain is the Key to Choosing the Right Probiotic
It’s become common knowledge that probiotics can help with gut function and digestive health – that’s perhaps what they are best known for. What you may not know though is your gut contains approximately 70% of your body’s immune system,[1] and knowing that, you may not be so surprised to hear that certain probiotics can influence the activity of your immune cells. So how do you know which ones these are?
First you need to understand that there are many different beneficial probiotics available and each one has a different role to play in human health.
As such, the way to make sure you are using the right probiotic for your needs is to check the specific genus, species and strain (see Figure 1) has been used in human clinical trials for the condition you want to use it for – in this case reducing the likelihood of you contracting a cold or flu – because not every probiotic would be indicated for this condition.
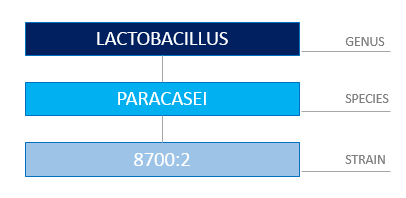
Figure 1: Correctly Identifying a Probiotic Requires You to Know the Genus, Species and Strain.
You may be wondering how a probiotic can enhance immune system function. To begin with, the microbial life living within your gastrointestinal tract (known as your gut microbiota) play an important role in maintaining the lining of your gut, which itself forms an intestinal defense barrier – so that’s one of the ways many probiotics can help – by supporting the health of the microbiota already residing within you.
However, certain probiotic strains have the ability to actually communicate directly with your immune cells, thus influencing and improving the immune response.[2]
Two of these probiotic strains are Lactobacillus rhamnosus (LGG®)[3] and Lactobacillus paracasei 8700:2,[4] both of which increase the activity of immune cells called natural killer (NK) cells – who, as their name suggest, actually target and kill virally infected cells – exactly what you want to tackle a cold or flu.
In addition, Lactobacillus paracasei 8700:2 and Lactobacillus plantarum HEAL 9 are two specific strains that stimulate other white blood cells (called ‘macrophages’) to secrete an important chemical signal that alerts your immune system to mount an antiviral immune response.[5],[6] Lastly, Lactobacillus plantarum HEAL 9, Lactobacillus paracasei 8700:2 and LGG® all have the capacity to trigger a natural chemical messenger inside your body called interleukin-10, which is a key anti-inflammatory and immune-regulating signal.[7],[8] Now that may all seem quite technical but what it helps demonstrate is that, used together, these three probiotic strains play a valuable role in supporting healthy immune system function.
Where’s the Evidence?
This isn’t all just theory; the ability of Lactobacillus plantarum HEAL 9 and Lactobacillus paracasei 8700:2 to improve immune function has been demonstrated in a randomised, controlled trial. Two hundred and seventy-two healthy adults were given 500 million CFU* each of Lactobacillus plantarum HEAL 9 and Lactobacillus paracasei 8700:2, or placebo, for 12 weeks. Those in the treatment group experienced fewer incidences of the common cold, with significantly reduced duration and symptom severity when infection did occur.[9] A combination of these two specific strains has also been shown to reduce symptom severity and duration of the common cold in subjects who are prone to recurrent infections.[10]
What this all tells you is these probiotic strains have actually been tested in real situations and shown to be helpful in not only preventing colds and flus but, when someone got sick, they reduced the numbers of sick days taken – essentially the people taking these probiotic strains recovered faster.
Prevention is Better Than Cure
Don’t wait until you get sick this year, or assume there is nothing you can do about it. If you have a history of frequent colds and flus (or maybe you were one of the people who succumbed to that debilitating flu that did the rounds in Australia in 2017), don’t just pop to the pharmacy and grab any probiotic; be strategic and speak to your Naturopath or other healthcare Practitioner first, and ask them how best to improve your immune surveillance with probiotic strains proven to enhance immunity.
You can also help support yourself by managing your stress levels (stress depletes your immune system), eating plenty of colourful vegetables and fruits, nuts and seeds (to improve your overall nutritional status – more on that in an upcoming blog post), and look after your gut health – remember, the gut is where much of your immune system is located. Take practical steps now to reduce the likelihood of you getting sick this winter, and enjoy the colder months healthy and well.
* CFU means ‘colony forming units’ and is what tells you these were live bacteria. Either CFU or ‘live bacteria’ are important things to look for on a probiotic label so you know the product contains viable organisms. Also – the specific strain must be listed on the label – if it is missing then don’t use the probiotic…you don’t know what it is!
References
[1] Gill HS. Probiotics to enhance anti-infective defences in the gastrointestinal tract. Best Practice and Research Clinical Gastroenterology. 2003;17(5):755-773.
[2] Lebeer S, Vanderleyden J, De Keersmaecker SC. Host interactions of probiotic bacterial surface molecules: comparison with commensals and pathogens. Nature Reviews Microbiology. 2010;8:171-184.
[3] Harata G, He F, Hiruta N, Kawase M, Kubota A, Hiramatsu M, et al. Intranasal administration of Lactobacillus rhamnosus GG protects mice from H1N1 influenza virus infection by regulating respiratory immune responses. Lett Appl Microbiol. 2010;50:597-602.
[4] Rask C, Adlerberth I, Berggren A, Ahren IL, Wold AE. Differential effect on cell-mediated immunity in human volunteers after intake of different lactobacilli. Clinical and Experimental Immunology. 2013;172(2):321-32.
[5] Rask C, Adlerberth I, Berggren A, Ahren IL, Wold AE. Differential effect on cell-mediated immunity in human volunteers after intake of different lactobacilli. Clinical and Experimental Immunology 2013;172(2):321-32.
[6] Leonard P, Sur S. Interleukin-12: potential role in asthma therapy. BioDrugs. 2003;17(1):1-7.
[7] Lavasani S, Dzhambazov B, Nouri M, Kak F, Buske S, Molin G, et al. A novel probiotic mixture exerts a therapeutic effect on experimental autoimmune encephalomyelitis mediated by IL-10 producing regulatory T cells. PLoS ONE. 2010;5(2):e9009.
[8] Feleszko W, Jaworska J, Rha RD, Steinhausen S, Avagyan A, Jaudszus A, et al. Probiotic-induced suppression of allergic sensitization and airway inflammation is associated with an increase of Tregulatory-dependent mechanisms in a murine model of asthma. Clin Exp Allergy. 2007;37(4):498-505.
[9] Berggren A, Lazou A, Larsson N, Onning G. Randomised, double-blind and placebo-controlled study using new probiotic lactobacilli for strengthening the body immune defence against viral infections. Eur J Nutr. 2011;50(3):203-210.
[10] Busch R, Gruenwald J, Dudek S. Randomised, double blind and placebo controlled study using a combination of two probiotic lactobacilli to alleviate symptoms and frequency of common cold. Food and Nutrition Sciences. 2013;4:13-20.
It’s not until your unwell🤒🤧🤕, that you realise…🍃
Did YOU KNOW?🤔🥂🥦🤦♀️🏃♀️💊
Microbiome 101
‘Microbiome’ is a hot topic right now for anyone interested in health; but you may be wondering what exactly it is? You’ve potentially heard about the good bacteria living within your digestive system, and may have even thought about taking a probiotic to support them. Well it’s this internal community – actually encompassing a massive 38 trillion microbes (not just bacteria) – that are collectively referred to as your commensal microbiome. When healthy and balanced, your microbiome has wide-reaching health effects, such as synthesising important vitamins you need; helping to modulate and boost your immune system; assisting with waste elimination (therefore supporting healthy bowel function); and even influencing your mood.1
However, your diet and lifestyle choices can negatively impact the health of your microbiome; resulting in a reduction in both the numbers and/or diversity of the organisms within your gut. Disruption to your internal microbial community can then create an environment where pathogenic (disease causing) organisms have the opportunity to grow and prosper. This state of imbalance is termed ‘dysbiosis’, and can lead to a plethora of negative health effects, including digestive complaints, nutrient deficiencies, or maybe a compromised immune system (which can lead to allergies and/or frequent illness) – these are all common outcomes when the microbiome becomes imbalanced.
The following are five of the most common diet and lifestyle factors that may negatively impact the health of your microbiome, along with some tips to help you re-establish a healthy and thriving microbial community once more.
Five ways you can upset your microbiome:
- Eating a low fibre diet: as your gut microbes rely on the fibre in your food for fuel, a low fibre diet leads to a reduction in the diversity of your microbiome.
Interestingly, evidence now shows those who consume more than 30 different types of plants/vegetables each week have a much more diverse microbiome compared to those who consume 10 or fewer types of plants weekly.2
- Alcohol intake: the consumption of alcohol can result in dysbiotic changes in your intestinal microbiome, and also triggers gastrointestinal inflammation.3 If you’re consuming more than one standard drink per day, your microbiome’s probably keen for you to abstain a bit more often!
- Unmanaged stress: when you are stressed, the release of the stress hormone cortisol, and adrenaline sensitise your body to inflammation, including gut inflammation.4 This disrupts the gut environment, compromising the conditions your beneficial microbes need to flourish.
- Leading a sedentary lifestyle: lack of exercise has also been linked to reduced microbial diversity in the gut – another reason to get moving!
- Antibiotic use: a round of antibiotics does lead to some loss of core commensal organisms (antibiotics are supposed to kill off bacteria however in this instance the good stuff goes too). This leaves the gut susceptible to microbiome imbalances and dysfunction. Due to this disruption, up to 10% of people experience gastrointestinal side effects5 from antibiotic use, referred to as antibiotic-associated diarrhoea (AAD).6,7
Do any of these situations apply to you? Fortunately, there are a few things you can do to support your microbiome and help correct any imbalance.

Fighting, Fixing and Fuelling
Addressing the five diet and lifestyle factors listed above is important for improving the health and diversity of your microbiome. Managing your stress levels, utilising antibiotics only when specifically needed (and taking stain-specific probiotic to restore your microbiome if you do), moderating your alcohol intake, and regularly exercising will all have your microbiome singing your praises! Additionally, and perhaps most importantly, consuming a diet rich in plant based fibres will provide ample fuel for your beneficial organisms to flourish. See Table 1 below for ideas on foods your microbiome loves.
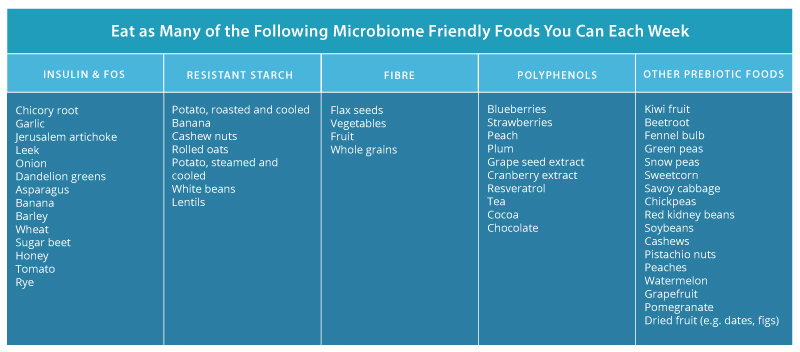
Table 1: Foods That Feed Your Microbiome
Nevertheless, there are situations where pathogenic organisms have the opportunity to establish within your gut and create dysbiosis, requiring specific natural formulations to address it. In this instance, antimicrobial herbal medicines can be employed, including pomegranate (Punica granatum),8 nigella (Nigella sativa),9 and myrrh (Commiphora myrrha).10, 11 These herbs work to eliminate unwanted organisms within the gut, and have even shown to be as effective as their pharmaceutical counterparts in helping to reduce pathogenic populations in scientific research.
However, while eliminating pathogenic species can begin to address an imbalanced microbiome, this is only one part of the puzzle. You also need to focus on regenerating and rebuilding the diversity of your commensal microbiome, which can be achieved with specific probiotic strains such as:
-
- Lactobacillus rhamnosus (LGG®): one of the most studied probiotic stains in the world, research shows LGG®administration to promote the growth and function of key core commensal bacteria.
- Saccharomyces cerevisiae (boulardii) (SB): multiple investigations have shown that boulardii reduces antibiotic-associated loss of bacteria, whilst also supporting the rapid restoration of the microbiome after antibiotic use.12
- Lactobacillus acidophilus (NCFM®)13 and Bifidobacterium animalis lactis (Bi-07): are two strains also highly indicated to protect and support a healthy microbiome.14

So whilst there are factors that can upset your microbiome, be assured there is also a multitude of natural medicines, diet and lifestyle options you can harness to encourage it’s health too, and hence the wellbeing of your whole body. Many of these tips are under your control, but if you feel you need some extra help and support with antimicrobial herbs and/or strain-specific probiotics talk to your healthcare Practitioner about a tailored microbiome-restoring treatment plan to suit your needs. Your beneficial bugs will thank you for it!
References
1. D’Argenio S. The role of the gut microbiome in the healthy adult status. Clinica Chimica Acta. 2015;451(Part A):97-102.
2. Buschman H, Bright D. Big Data from World’s Largest Citizen Science Microbiome Project Serves Food for Thought. [Internet]. San Diego (CA): UC San Diego School of Medicine. 2018 [cited 2018 July 05]. Available from: https://health.ucsd.edu/news/releases/Pages/2018-05-15-big-data-from-worlds-largest-citizen-science-microbiome-project-serves-food-for-thought.aspx
3. Engen PA, Green SJ, Voiqt RM, Forsyth CB, Keshavarzian A. The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota. Alcohol Res. 2015;37(2):223-36.
4. Guilliams TG. The role of stress and the HPA axis in chronic disease management. Point Institute, Stevens point (WI). 2015;80.
5. NPS Medicinewise. What are the side effects of antibiotics? [Internet]. Sydney NSW: NPS Medicinewise; 2012 [updated 2017 Mar; cited 2018 July 05]. Available from: http://www.nps.org.au/medicines/infections-and-infestations/antibiotics/for-individuals/side-effects-of-antibiotics.
6. Eloe-Fedrosh E, Brady A ,Crabtree J, Drabek E, Ma B, Mahurkar A, et al. Functional dynamics of the gut microbiome in elderly people during probiotic consumption. M Bio. 2015 Apr 14;16(2):e00231-15.
7. McFarland L. Use of probiotics to correct dysbiosis of normal microbiota following disease or disruptive events: a systematic review. BMJ Open. 2014 Aug 25;4(8):e005047.
8. Abdel-Haffez E, Ahmed A, Abdellatif M, Kamal A, Toni N. The efficacy of pomegranate (Punica granatum) peel extract on experimentally infected rats with blastocystis spp. J Infect Dis Preve Med. 2016;4(1):1-6.
9. Salem EM, Yar T, Bamosa AO, Al-Quorain A, Yasawy MI, Alsulaiman RM, et al. Comparative study of Nigella sativa and triple therapy in eradication of Helicobacter pylori in patients with non-ulcer dyspepsia. Saudi J Gastroenterol. 2010 Jul;16(3):207.
10. Fathy FM. Effect of mirazid (Commiphora molmol) on experimental giardiasis. J Egypt Soc Parasitol. 2011 Apr;41(1):155-77.
11. Basyoni MM, El-Sabaa AA. Therapeutic potential of myrrh and ivermectin against experimental Trichinella spiralis infection in mice. Korean J Parasitol. 2013 Jun;51(3):297-304. doi: 10.3347/kjp.2013.51.3.297.
12. Moré M, Swidsinski A. Saccharomyces boulardii CNCM 1-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis – a review. Clinical and Experimental Gastroenterology. 2015;8:237-55.
13. Anderson JM, Barrangou R, Hachem MA, Lahtinen SJ, Goh YJ, Svensson B, et al. Transcriptional analysis of prebiotic uptake and catabolism by Lactobacillus acidophilus NCFM. PLos ONE. 2012;7(9):e44409.
14. Mäkeläinen H, Saarinen M, Stowell J, Rautonen N, Ouwehand AC. Xylo-oligosaccharides and lactitol promote the growth of Bifidobacterium lactis and Lactobacillus species in pure cultures. Benef Microbes. 2010 Jun;1(2):139-48