

![]()
This is what goes on inside the body when we are chronically stressed
How stress affects your body – Sharon Horesh Bergquist
Let’s Begin…

If this is you… it’s time to get some help!😱😴
Turmeric! Are you taking an effective dose?🤔🍃
Nature’s Cure-Alls
In the late 1950s and 60s, it was not uncommon for a daily dose of foul-tasting, fishy smelling liquid to be forced upon sickly children by their grandparents and cited as the cure for everything from arthritis and baldness, to boils and piles. Cod liver oil consumption was at its peak, simultaneously torturing yet improving the health of children and their families all over the world. In the decades that followed various other natural remedies came in and out of the limelight. Apricot seed kernels, goji berries and coconut oil all enjoyed their glory days – with some developing a near cult following. However, as time passed and science accumulated (or failed to accumulate), it became clear that these natural remedies weren’t really the ‘cure all’ they were sometimes promoted to be. In recent years, another natural medicine has forged ahead as the latest trendy cure-all taking the population by storm; yet this one has the scientific backing to boot.
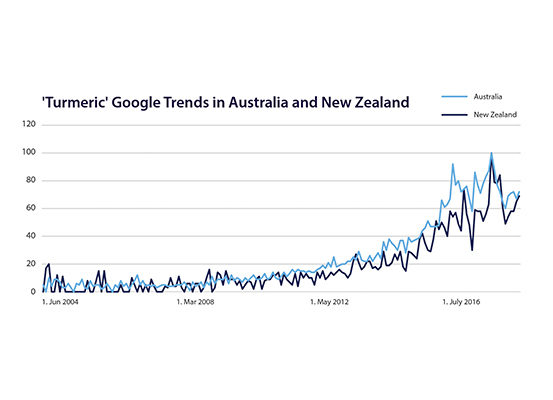
Figure 1a. Turmeric is Trending Amongst Consumers. Google Trends Showing the Public Interest in ‘Turmeric’ in Australia and New Zealand.
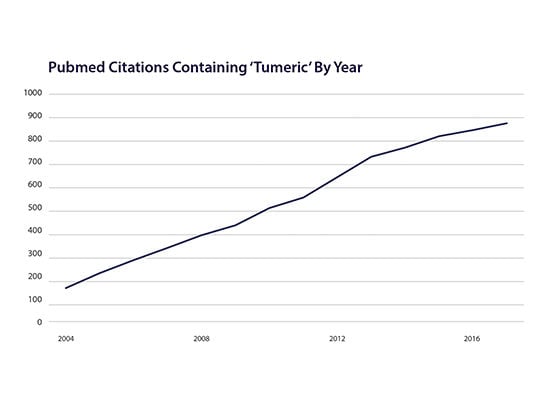
Figure 1b. Turmeric is Trending in Research. PubMed Citations Containing ‘Turmeric’ by Year.
A Condiment and a Cure
The cultural and medicinal history that surrounds turmeric is one that transcends time. Used for at least 6000 years in traditional medicine, food preparation and religious practice, it was long considered to be a sacred harbinger of prosperity amongst many Indian communities. Today, a cascade of promising studies have verified the value it brings. Developing a strong reputation as an anti-inflammatory and antioxidant early on, turmeric now boasts over 7500 scientific publications, which show it benefits a huge array of health conditions: arthritis1,2 cardiovascular disease,3 Alzheimer’s disease4 improved oral hygiene;5 it even has anti-ageing properties. You name the ailment, there is a good chance turmeric has been indicated to be of benefit – and that what you’ve heard is true. Unsurprisingly, all of these emerging health applications have roused a huge love affair with turmeric which has seen turmeric supplements prosper commercially, almost doubling sales within a year.6 However, like all great love affairs it is not without some challenges, and emotional baggage.
Curcumin – Just One Part of a Whole
First isolated in 1815, curcumin, the constituent that gives turmeric its yellow colour, takes much of the credit for the overall benefits of turmeric. This has led to the influx of several isolated curcumin supplements onto the natural medicines market. However, as the wise Greek philosopher Aristotle once proclaimed, the benefits of the whole herb is much greater than the sum of its parts, or more specifically, than one part alone. Certainly, curcumin is a gifted compound however, the whole turmeric root also provides resins and other volatile oils such as turmerones which offer additive anti-inflammatory,7 antimicrobial8 and anticancer9 effects. The first challenge when selecting the most appropriate turmeric supplement to engage in a relationship with, is to ensure you opt for the whole herb (i.e. the label reads Curcuma longa – Turmeric) to achieve the best outcomes; as using curcumin alone limits its therapeutic potential.
Turmeric’s Emotional Baggage
What many don’t realise is, regardless of whether you select the whole turmeric or curcumin alone, another major relationship conundrum remains: the compound curcumin (which comes with both) has notoriously poor bioavailability, meaning, it has low absorption and uptake into the body (aka the emotional baggage) (Figure 2).10 In fact, several animal studies have shown that as much as 90% of oral curcumin is excreted (from the other end). Drinking your daily turmeric latte and having the occasional Indian takeaway, therefore, could be giving you a false sense of security – that you’re obtaining all the potential health gains from this extraordinary herb, however you may not actually be absorbing sufficient levels. Turmeric supplements help overcome this relationship hurdle by providing concentrated extracts, which far exceed even the most impressive dietary intakes of curry. That said, absorption issues still need to be addressed, something that every manufacturer of Turmeric supplements is aware of.
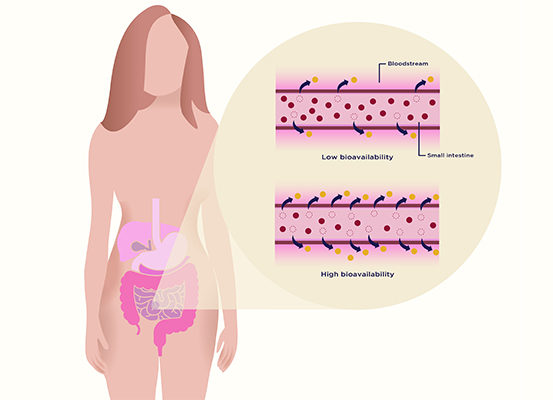
Figure 2: Bioavailability Refers to How Well Something Can be Absorbed and Used by Your Body.
The Turmeric Arm’s Race
In response to the analyses proving poor turmeric absorption, a competitive buzz has been generated amongst supplement manufacturers who strive to meet the challenges of this talented yet temperamental therapy. Hi-tech, impressive-sounding bioavailability technologies such as nanoparticles, liposomes, micelles and phospholipid complexes – anything which can get it out of the intestines and into the blood as efficiently as possible – are constantly being evaluated and promoted to health professionals and consumers alike.11 Fortunately, the whole herb does enhance curcumin absorption thanks to the addition of the volatile oils. Many of the other options are heavily reliant on additives to perform, and as one tablet can only fit so many ingredients before it becomes a ‘horse-pill’, this often comes at the expense of the curcumin content itself. It is also very difficult to evaluate which technology is the leader in this turmeric arm’s race. Head-to-head studies directly comparing the different technologies are sparse, and they use different methodologies to assess absorption – so for the most part it can be like comparing apples with oranges. To throw another spanner in the works, the latest science on turmeric is showing that while bioavailability is likely important, it may not be the sole or even primary factor that determines its effectiveness. That’s because the time turmeric spends in the digestive tract contributes to its health benefits across all systems of the body – including the joints, heart and brain.
Health Begins in the Gut
Perhaps the single most recited quote amongst natural medicine circles is that from Hippocrates: “all disease begins in the gut.” Sharing this wisdom over 2000 years ago, we now have scientific confidence that truer words have never been spoken. The surface area of the inner lining of the digestive tract is thought to be roughly the size of a studio apartment12 – and even though it technically sits inside of our body, it acts as the primary interface with our outside environment. Not only is it a direct physical barrier protecting against entry from the constant assault of inflammatory toxins, dietary antigens, and microbes (like bacteria), it houses more nerves than the rest of our nervous system put together, and directs more immune decisions in one day than the entire immune system makes in a lifetime. In addition to this impressive resume, it is also home to a more than a 90% share of the human microbiome (the microbes that live on us and in us) – which in the last decade has proven to be intimately connected with all aspects of human health.
It comes as no surprise that weakening of the gut barrier, sometimes referred to as ‘leaky’ gut (meaning inflammatory compounds can leak into the blood stream), and disruption of the levels of the gut’s microbial inhabitants, has been linked to almost every known health disorder. This includes digestive conditions, autoimmune disease, allergies, metabolic dysfunction, and mental health imbalances such as depression.13,14 Interestingly, turmeric has been shown to benefit many of these conditions.
The New Age Antidepressant
To isolate just one example, Australia’s very own psychologist and researcher Dr Adrian Lopresti, has published several impressive studies, finding the specific extract BCM-95™ Turmeric, when taken alone and in combination with the herb saffron, improves symptoms of major depression.15 There are multiple mechanisms to explain how it helps, but of most significance is its ability to reduce inflammation and increase protective compounds within brain regions that have been implicated in depression16,17 Yet again, it is not just the curcumin, but tumerones found within the whole herb that contribute to its antidepressant activity.18 While we’ve concluded that many of these actions are reliant on turmeric’s systemic tissue distribution, our assumptions may have been slightly misguided.
Exciting new evidence over the past decade has identified strong links between depression, changes in the microbiome, and a leaky gut; with inflammation thought to play the key intermediary role. Hence, reducing gut inflammation is a key therapeutic target for depression, and many other conditions as well. Conceivably, it is this mechanism through which turmeric works.
The Gut Loves Curry
Although the research is still in its infancy, studies suggest that the system-wide medicinal benefits of turmeric are, at least in part, mediated through its ability to correct both gut barrier integrity and microbiome disturbances – local gastrointestinal actions that are not reliant on its absorption (Figure 3). Turmeric interventions have been shown to increase the activity of genes which promote gut barrier healing, and offset the negative effects of drugs known to significantly damage the gut barrier.19 In addition to improving barrier integrity, turmeric targets the gut microbes, increasing their richness and diversity – markers of a healthy gut microbiome.20 The net effect is reduced inflammation within the gastrointestinal tract and throughout the entire body – producing body-wide health benefits. These combined actions may not render the question around turmeric absorption obsolete, but highlight the limitations of focusing on bioavailability alone. Simply put, turmeric extracts may not necessarily need high bioavailability to be a highly effective health remedy. So, how do you choose the right turmeric for you? Opt for extracts that produce the most impressive results when trialed in humans for the condition that you are taking turmeric for. For example, BCM-95™ is a great option for depression, and has also produced impressive results for osteoarthritis and rheumatoid arthritis. If you are not sure how to interpret clinical data yourself, speak to your naturopath or a Healthcare Practitioner who can. One thing we can predict with high probability, turmeric will continue to be trusted, loved and respected as a golden example of the benefits of natural therapies.
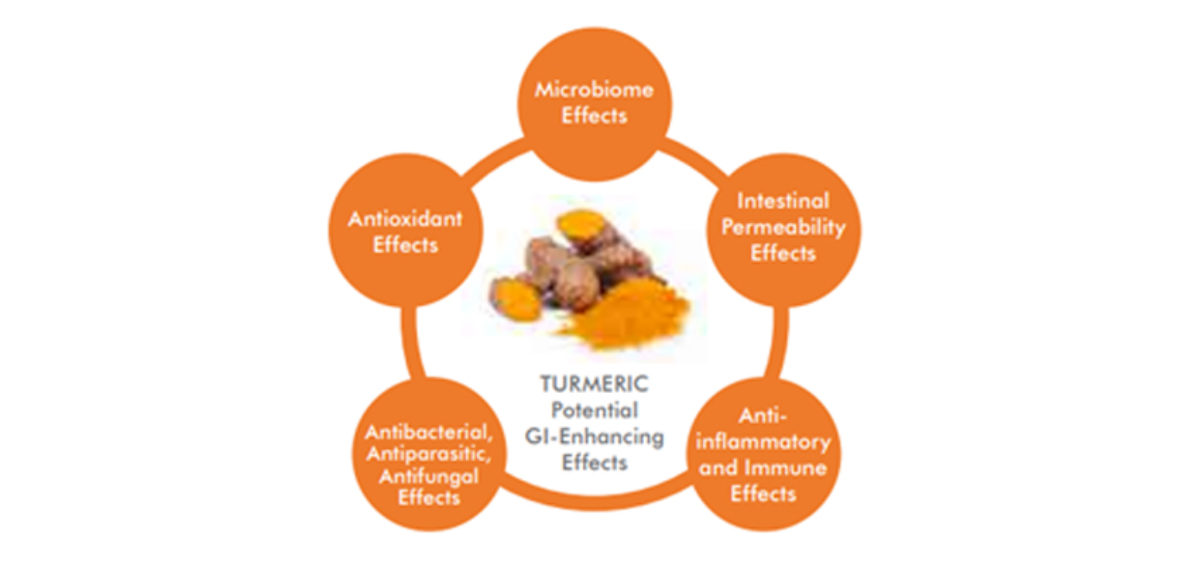
Figure 3: Potential Gastrointestinal-Enhancing Effects of Turmeric that May Contribute to its Systemic Health Effects.
References
1. Horayan A, Mukuchyan V, Mkrtchyan N, Minasyan N, Gasparvan S, Sargsyan A, et al. Efficacy and safety of curcumin and its combination with boswellic acid in osteoarthritis: a comparative randomised, double-blind, placebo-controlled study. BMC Complementary and Alternative Medicine. 2018;18(1)7. doi: 10.1186/s12906-017-2062-z.
2. Chandran B, Goel A. A randomized pilot study to assess the efficacy and safety of curcumin in patients with active rheumatoid arthritis. Phytotherapy Research. 2012 26(11): 1719-25.
3. Hewlings S, Kelman D. Curcumin: a review of it’s effect on human health. Foods. 2017 Oct 22;6(10). doi: 10.3390/foods6100092.
4. Mirmosayyeb O, Tanhaei A, Sohrabi HR, Martins RN, Tanhaei M, Najafi MA, et al. Possible Role of Common Spices as a Preventive and Therapeutic Agent for Alzheimer’s Disease. Int J Prev Med. 2017 Feb 7;8:5. doi: 10.4103/2008-7802.
5. Pulikkotil SJ, Nath S. Effects of curcumin on crevicular levels of IL-1β and CCL28 in experimental gingivitis. Aust Dent J. 2015 Sep;60(3):317-27
6. Natural Products Insider. 2016;6(14).
7. Del Prete D, Millan E, Pollastro F, Chianese G, Luciano P, Collado JA, et al. Turmeric Sesquiterpenoids: Expeditious Resolution, Comparative Bioactivity, and a New Bicyclic Turmeronoid. J Nat Prod. 2016 Feb 26;79(2):267-73. doi: 10.1021/acs.jnatprod.5b00637
8. Prasad S, Gupta SC, Tyagi AK, Aggarwal BB. Curcumin, a component of golden spice: from bedside to bench and back. Biotechnol Adv. 2014;32:1053–1064.
9. Tyagi AK, Prasad S, Yuan W, Li S, Aggarwal BB. Identification of a novel compound (β-sesquiphellandrene) from turmeric (Curcuma longa) with anticancer potential: comparison with curcumin. Invest New Drugs. 2015 Dec;33(6):1175-86.
10. Burgos-Morón E, Calderón-Montaño JM, Salvador J, Robles A, López-Lázaro M. The dark side of curcumin. Int J Cancer. 2010;126:1771-5
11. Prasad S, Gupta SC, Tyagi AK, Aggarwal BB. Curcumin, a component of golden spice: From bedside to bench and back. Biotechnol Adv. 2014;32:1053-64.
12. Helander HF, Fändriks L. Surface area of the digestive tract – revisited. Scandinavian Journal of Gastroenterology. 2014 Jun;49(6):681-9. doi: 10.3109/00365521.2014.898326.
13. Lloyd-Price J, Abu-Ali G, Huttenhower C. The healthy human microbiome. Genome Med. 2016;8:51.
14. Amalraj A, Pius A, Gopi S, Gopi S. Biological activities of curcuminoids, other biomolecules from turmeric and their derivatives – A review. J Tradit Complement Med. 2017 Apr;7(2):205–233.
15. Lopresti AL, Maes M, Maker GL, Hood SD, Drummond PD. Curcumin for the treatment of major depression: a randomised, double-blind, placebo controlled study. J Affect Disord. 2014;167:368-75.
16. Pereira Dias G, Cavegn N, Nix A, do Nascimento Bevilaqua M, Stangl D, Zainuddon M, et al. The Role of Dietary Polyphenols on Adult Hippocampal Neurogenesis: Molecular Mechanisms and Behavioural Effects on Depression and Anxiety. Oxid Med Cell Longev. 2012;2012:541971.
17. Xu Y, Ku B, Tie L, Yao H, Jiang W, Ma X, et al. Curcumin reverses the effects of chronic stress on behavior, the HPA axis, BDNF expression and phosphorylation of CREB. Brain Res. 2006 Nov 29;1122(1):56-64. Epub 2006 Oct 3.
18. Lopresti A. The Problem of Curcumin and Its Bioavailability: Could Its Gastrointestinal Influence Contribute to Its Overall Health-Enhancing Effects? Advances in Nutrition. 2018;9(1):41-50.
19. Lopresti A. The Problem of Curcumin and Its Bioavailability: Could Its Gastrointestinal Influence Contribute to Its Overall Health-Enhancing Effects? Advances in Nutrition. 2018;9(1):41-50.
20. Lopresti A. The Problem of Curcumin and Its Bioavailability: Could Its Gastrointestinal Influence Contribute to Its Overall Health-Enhancing Effects? Advances in Nutrition. 2018;9(1):41-50.
21. Adapted from: Lopresti A. The Problem of Curcumin and Its Bioavailability: Could Its Gastrointestinal Influence Contribute to Its Overall Health-Enhancing Effects? Advances in Nutrition. 2018;9(1):41-50
STRESS! A key factor in creating MENOPAUSE Symptoms.🤯 Time to put YOURSELF FIRST!🍃🙏💞

Menopause is a natural process where a woman transitions from her childbearing years to the next stage of her life. Whilst menopause usually occurs around age 50, a woman is said to be officially in menopause once she has not had a menstrual period for twelve consecutive months so this can occur at various ages. However, for many women, the months or years leading into menopause (known as perimenopause), can mark the onset of challenging symptoms including irregular menstrual cycles, flushing sensations, irritability and night sweats.
So what is actually happening within a woman’s body during menopause? Firstly, the ovaries stop producing hormones, particularly oestrogen, which results in the cessation of the menstrual period. You still need some oestrogen for important non-reproductive functions such as supporting bone health, therefore many other tissues including the brain, adrenal glands, and adipose (fat) tissue actually continue the role of oestrogen production for the remainder of a woman’s life, which begins to reveal why some woman experience menopause differently to others. What this means is – what impacts these tissues, impacts your symptoms.

Is it Getting Hot in Here or Is It Just Me?
Up to 80% of peri- and postmenopausal women report having vasomotor symptoms (VMS), such as hot flushes and night sweats; with up to half of these women reporting moderate or severe symptoms.1 The drop in oestrogen that naturally occurs in menopause is seen to be a significant culprit for hot flushes, however it is not the only cause. As similar levels of circulating oestrogen are found in women with and without VMS symptoms, this indicates other factors are at play.2
Remarkably, menopausal hot flushes are a result of the brains perception of temperature, due to the narrowing or reduction in something called the thermoneutral zone. Normal variations in body temperature within this zone means the body does not have to start shivering to warm up, or sweat to cool down. However, in menopause, the narrowing of this zone means that any slight elevation in temperature then triggers the sweating and flushing response, as the brain perceives the body’s temperature to be too hot.
As further proof of this, women experiencing menopausal flushes are not actually hotter in temperature than people not experiencing flushing – how fascinating!
Whilst declining oestrogen is one of the reasons for the narrowing of this zone, it is not the only cause. In fact, it is stress levels that play a larger role than oestrogen levels in triggering hot flushes. To highlight this, recent research has found that menopausal women have increased activity of the stress centre of the brain right before the onset of a hot flush.3
Therefore, it is vitally important to support a healthy stress response, not just hormones, to reduce menopausal symptoms.
Ingredients to Support Your Stress Response
The good news is that specific herbs and nutrients can support and nourish your stress response, and hence support your menopausal symptoms. Such ingredients include:
- B vitamins: as they have an increased demand during stressful times, with vitamins B5 and B6 especially required by your adrenal glands to synthesis their hormones. If a woman has a narrowed thermoneutral zone due to stress, and is hence experiencing VMS symptoms, B vitamins will help the adrenals function optimally.
- Magnesium: is a mineral that your body increases the elimination of when stressed, but is actually needed to calm the stress response. Therefore, supplying magnesium helps decrease your body’s sensitivity to stress, and as a bonus it helps improve energy levels. To learn more about the wonders of magnesium for hormonal conditions, read this blog.
- Rehmannia Six: a traditional Chinese medicine herbal combination that has been used for centuries to treat night sweats, anxiety and insomnia, making this an ideal formulation to discuss with your Practitioner for reducing symptoms associated with menopause. The influences of these herbs on the thermoneutral zone were demonstrated in a clinical trial on menopausal women, with the Rehmannia Six combination significantly reducing hot flushes and sweating.4
Time to Put Yourself First
Now you know that stress is a key factor creating menopause symptoms, it’s no surprise that your lifestyle plays a fundamental role in helping you sail through this life transition.
Research shows that mind-body therapies, such as yoga, tai chi, mindfulness, meditation, cognitive behavioral therapy and aerobic exercise improve overall menopausal symptoms, such as flushing, night sweats, insomnia and mood changes.5
Further, 65% of postmenopausal woman are classified as obese. Therefore, moving your body using the above methods will help to not only lose weight but also improve your symptoms, with evidence showing weight loss alone to be enough for some women to reduce their hot flushes.6
In this transitional time for women, it’s important to examine your stress levels, review your current lifestyle choices, and establish healthy habits. Remember, hormones are one part of the picture in menopause, but they aren’t the only contributor. Your whole body is made of many complexities, and addressing all aspects that influence your menopausal symptoms is vital when embarking on this next stage of life. For tailored support with your journey towards a balanced and vibrant body, click here to find your closest natural medicine Practitioner today.
References
1. Chiaramonte D, Ring M, Locke AB. Integrative Women’s Health. Med Clin North Am. 2017 Sep;101(5):955-975. doi: 10.1016/j.mcna.2017.04.010.
2. Freedman RR. Menopausal hot flashes: Mechanisms, endocrinology, treatment. J Steroid Biochem Mol Biol. 2014 Jul;142:115-20.
3. Diwadkar VA, Murphy ER, Freedman RR. Temporal sequencing of brain activations during naturally occurring thermoregulatory events. Cereb Cortex. 2014 Nov;24(11):3006-13. doi: 10.1093/cercor/bht155.
4. Zhang JP, Zhou DJ. Changes in leucocytic estrogen receptor levels in patients with climacteric syndrome and therapeutic effect of liuwei dihuang pills.Zhong Xi Yi Jie He Za Zhi. 1991 Sep;11(9):521-3,515. PMID: 1773463.
5. Goh VHH, Hart WG. Excess fat in the abdomen but not general obesity is associated with poorer metabolic and cardiovascular health in premenopausal and postmenopausal Asian women. Maturitas. 2018 Jan;107:33-38. doi: 10.1016/j.maturitas.2017.10.002
6. Thurston RC, Ewing LJ, Low CA, Christie AJ, Levine MD. Behavioral weight loss for the management of menopausal hot flashes: a pilot study. Menopause. 2015 Jan;22(1):59-65. doi: 10.1097/ GME. 0000000000000274.
Have you started on your health journey?🍃

If your busy lifestyle leaving you feeling tired, stressed and out of balance?
Do You Need More Magnesium?
While stress is a key culprit in reducing magnesium, there are other factors which can diminish levels of this vital mineral including reproductive hormonal changes (e.g. pregnancy) and long-term use of the oral contraceptive pill.3
Further, modern food processing techniques can contribute to a reduction of dietary magnesium consumed.4 If you are one of the many women with hormonal complaints such as premenstrual syndrome (PMS),5 menstrual migraine,6 polycystic ovarian syndrome (PCOS)7 and symptomatic menopause;8,9 your magnesium levels may be 20-30% lower than those who are symptom free.
For more on hormonal conditions read this article.
That’s not all though. Many women turn to coffee and/or alcohol as a way of raising energy or ‘winding down’; however, research shows an excess intake of these can also deplete magnesium levels.10 If this is you, it may well be time to explore some new invigorating or stress management strategies, such as swapping out one of your fitness classes for some restorative yoga, or perhaps a regular walk in nature.
How Stress Wields a Hefty Blow
Even if you don’t feel stressed, the persistent busyness of everyday life is still seen as a type of stress which can take its toll on your body. The ‘stress response’ causes the adrenal glands to release hormones (e.g. cortisol) and neurotransmitters (messenger molecules such as adrenaline, noradrenaline, and a small amount of dopamine). However, this leads to magnesium being released from your cells, and excreted via the urine, lowering levels and amplifying the stress response.11 Essentially, whilst you have an increased demand for magnesium when you are stressed, your body offloads it when you need it most! This vicious cycle can leave you low in magnesium, with flow-on effects on healthy nervous system function and hormonal balance.
The Magic of Magnesium for Female Health

Whilst the mechanisms impacting magnesium levels may seem complex (and maybe alarming!), the solution is actually very simple – focus on incorporating foods rich in magnesium into your daily diet (e.g. dark green leafy veg, quinoa, almonds, and black beans are all options); plus you can rapidly replenish your magnesium levels through quality supplementation. This way you can support a healthy stress response, but also help tackle any premenstrual migraines, period pains, and/or mood symptoms (e.g. mood swings, irritability, anxiety).12
Moreover, magnesium supplementation can help manage conditions such as endometriosis and fibroids, by supporting healthy oestrogen metabolism and clearance,13,14,15 therefore helping restore balance.
Interestingly, magnesium also helps to prevent bone loss approaching menopause, by reducing the inflammation and free radical damage that can drive bone deterioration occuring post-menopausally.16 As you can see, virtually all women could benefit from magnesium at some point in their lives.
Which Form of Magnesium is the Best?
This is an understandable question with so many to choose from, and important as not all forms of magnesium are equal. Look for amino acid chelates, such as magnesium bisglycinate (e.g. Meta Mag®). This has a unique biochemical shape that makes it the most effectively absorbed form of magnesium,17,18 which is what you want – magnesium getting to the areas of your body where it is needed most, so you can feel it’s effects.
If you have hormonal symptoms (such as PMS or period pain), magnesium works well alongside:
- Boswellia: a herb with potent anti-inflammatory and analgesic effects19 to reduce PMS symptoms and period pain;
- Chromium: alleviates cravings associated with PMS;20
- Chamomile: helps relieve stress, calms, and supports healthy mood;21 and
- Broccoli: aids in the elimination of hormone-disrupting environmental chemicals.22,23 (This topic was discussed in an earlier blog.)
As navigating hormonal conditions can be tricky – speak to a natural healthcare Practitioner for the most appropriate solution for your needs for best results.
Create a Life of Hormonal Bliss
Stress management is an essential part of enjoying healthy hormonal balance, but there is more you can do. Take a holistic perspective and support your overall health by engaging in regular physical activity, drinking 1-2 litres of water daily, and ensuring your diet is rich in ‘good’ fats such as avocado, oily fish (e.g. salmon, anchovies, mackerel), and nuts and seeds (your body requires good fats to make hormones).
Busy woman have better things to do than spend time curled up in bed with period pain, or inconvenienced by some other hormonal symptom. If this is you, begin today to turn things around by ensuring you have your stress under control, and speaking to your Practitioner about your need for magnesium (or about any other health related questions you may have) so you can continue to take on the world happy and healthy!
References
1. Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. 2011 Jan;15(1):18-22.
2. Eby GA 3rd, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010 Apr;74(4):649-60.
3. Eby GA 3rd, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010 Apr;74(4):649-60.
4. Eby GA 3rd, Eby KL. Magnesium for treatment-resistant depression: a review and hypothesis. Med Hypotheses. 2010 Apr;74(4):649-60.
5. Abraham GE, Lubran MM. Serum and red cell magnesium levels in patients with PMT. Am J Clin Nutr. 1981;34:2364-6. doi: 10.1093/ajcn/34.11.2364.
6. Mauskop A, Altura BT, Altura BM. Serum ionized magnesium levels and serum ionized calcium/ionized magnesium ratios in women with menstrual migraine. Headache. 2002 Apr;42(4):242-8. PMID: 12010379.
7 Chakraborty P, Ghosh S, Goswami SK, Kabir SN, Chakravarty B, Jana K. Altered trace mineral milieu might play an aetiological role in the pathogenesis of polycystic ovary syndrome. Biol Trace Elem Res. 2013 Apr;152(1):9-15. doi: 10.1007/s12011-012-9592-5.
8. López-González B, Molina-López J, Florea DI, Quintero-Osso B, Pérez de la Cruz A, Planells del Pozo EM. Association between magnesium-deficient status and anthropometric and clinical-nutritional parameters in postmenopausal women. Nutr Hosp. 2014 Mar 1;29(n03):658-664. doi: 10.3305/nh.2014.29.3.7198.
9. Okyay E, Ertugrul C, Acar B, Sisman AR, Onvural B, Ozaksoy D. Comparative evaluation of serum levels of main minerals and postmenopausal osteoporosis. Maturitas. 2013 Dec;76(4):320-5. doi: 10.1016/j.maturitas.2013.07.015.
10. Johnson S. The multifaceted and widespread pathology of magnesium deficiency. Med Hypotheses. 2001 Feb;56(2):163-70.
11. Cuciureanu MD, Vink R. Magnesium and stress. In: Vink R, Nechifor M. Magnesium in the central nervous system. Adelaide: University of Adelaide Press; 2011. p. 251-268.
12. Parazzini F, Di Martino M, Pellegrino P. Magnesium in the gynaecological practice: a literature review. Magnes Res. 2017 Feb 1;30(1):1-7. doi: 10.1684/mrh.2017.0419.
13. Brown RC, Bidlack WR. Dietary magnesium depletion: p-nitroanisole metabolism and glucuronidation in rat hepatocytes and hepatic microsomal membranes. Proc Soc Exp Biol Med. 1991 May;197(1):85-90. PMID: 1902295.
14. Maruti SS, Li L, Chang JL, Prunty J, Schwarz Y, Li SS, et al. Dietary and demographic correlates of serum beta-glucuronidase activity. Nutr Cancer. 2010;62(2):208-19. doi: 10.1080/01635580903305375.
15. Balthazart J, Baillien M, Charlier TD, Cornil CA, Ball GF. Multiple mechanisms control brain aromatase activity at the genomic and non-genomic level. J Steroid Biochem Mol Biol. 2003 Sep;86(3-5):367-79. PMID: 14623533.
16. Castiglioni S, Cazzaniga A, Albisetti W, Maier JA. Magnesium and osteoporosis: current state of knowledge and future research directions. Nutrients. 2013 Jul 31;5(8):3022-33. doi: 10.3390/nu5083022.
17 Albion Human Nutrition. Magnesium: Clinical and health benefits still without limits. Albion Research Notes. 2003 Oct;12(3):1-4.
18. Siebrecht S. Magnesium bisglycinate as safe form for mineral supplementation in human nutrition. Int J Orthomol Rel Med. 2013;144:1-16.
19. Sharma A, Bhatia S, Kharya MD, Gajbhiye V, Ganesh N, Namdeo AG, et al. Anti-inflammatory and analgesic activity of different fractions of Boswellia serrata. Int J Phytomed. 2010;2(1). doi: 10.5138/ijpm.2010.0975.0185.02015.
20. Brownley KA, Girdler SS, Stout AL, McLeod MN. Chromium supplementation for menstrual cycle-related mood symptoms. J Diet Suppl. 2013 Dec;10(4):345-56.
21. Amsterdam JD, Li Y, Soeller I, Rockwell K, Mao JJ, Shults J. A randomized, double-blind, placebo-controlled trial of oral Matricaria recutita (chamomile) extract therapy for generalized anxiety disorder. J Clin Psychopharmacol. 2009 Aug;29(4):378-82.
22. Boddupalli S, Mein JR, Lakkanna S, James DR. Induction of phase 2 antioxidant enzymes by broccoli sulphoraphane: perspectives in maintaining the antioxidant activity of vitamins A, C, and E. Front Genet. 2012 Jan 24;3-7. doi: 10.3389/fgene.2012.00007.
23. Riedl MA, Saxon A, Diaz-Sanchez D. Oral sulphoraphane increases Phase II antioxidant enzymes in the human upper airway. Clin Immunol. 2009;130: 244–25. doi: 10.1016/j.clim.2008.10.007.
Do the highs and lows of (PMS), pelvic pain or heavy flow hamper normal functioning around the time of your period?🤪🤯🤦♀️
Oestrogen is predominately thought of as a female hormone; but just as women have small amounts of the male hormone, testosterone – men also need some oestrogen (albeit at lower levels) for optimal health.
Oestrogen wears many hats, and they’re not all related to reproduction!
It also supports brain health. For example, it has been linked to slowing down the ravages of ageing and is protective against many neurological conditions such as Alzheimer’s disease, schizophrenia and depression.1 Oestrogen is also considered the beauty hormone; she plays a role in collagen production and moisture retention for supple skin,2 helping you looking more youthful! She is part of the reason why women retain hair on their heads, but have thinner hair elsewhere on the body. Oestrogen will also help bones remain strong by preventing calcium loss, and even supports healthy cholesterol metabolism (see Figure 1).
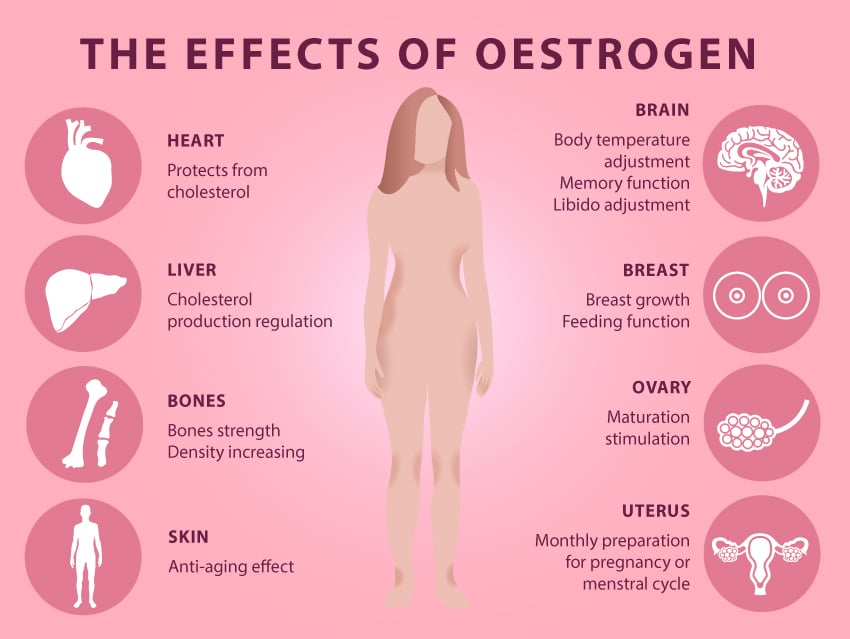
Figure 1: The Many Effects of Oestrogen.
All that said, oestrogen’s primary function is as a reproductive hormone. Levels begins to increase in young girls in puberty, around the time their periods begin. It is produced mainly by the ovaries, and will go on to shape and grow the breasts, the uterus and it’s lining (known as the endometrium) – essentially preparing the female body for reproduction. Interestingly, males also rely on oestrogen for the all-important task of creating healthy sperm!
Fun Fact: Did you know that during pregnancy, oestrogen levels are 1000 times higher than in non-pregnant women? This increase helps to expand the uterus to make space for the developing foetus and prepares the breasts for lactation.3
Intracrinology – Intra What?
I know I mentioned earlier that oestrogen is produced primarily by the ovaries but this sneaky hormone can also be synthesised in other tissues in the body including the breast, the brain and even in body fat! Known as the science of intracrinology, the study of hormone levels in different tissues can give some fascinating insights into the activity of oestrogen throughout the body. As shown in Figure 2 below, many factors (such as increased production in various tissues and impaired detoxification) can disrupt the delicate balance of hormones and in some cases lead to having too much.
Excess oestrogen may result in symptoms such as period pain, heavy flow, PMS and even more serious presentations such as endometriosis,4 fibroids5 and breast cancer.6
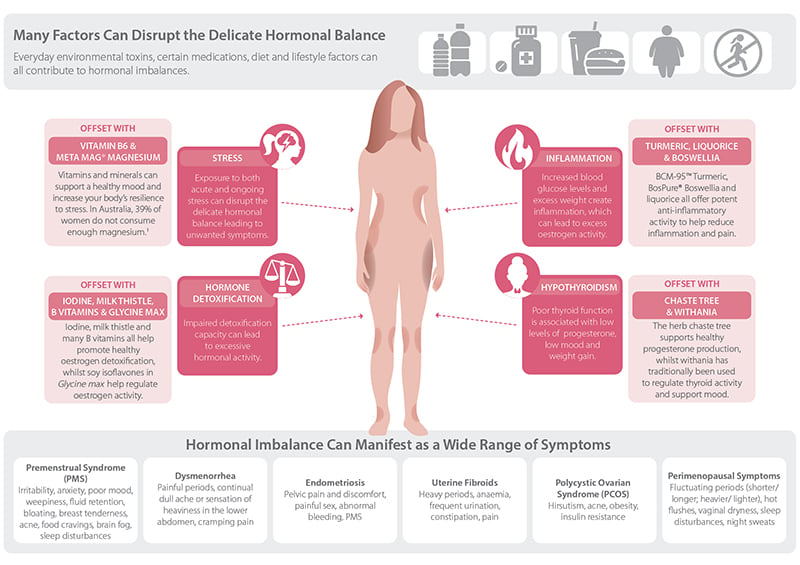
Figure 2: Many Factors Can Disrupt Hormonal Balance, But There Are Things You Can do to Correct This.
To give another example – if a woman is overweight, the extra fatty tissue can hold more oestrogen in the body, which can potentially lead to oestrogen excess and a worsening of hormonal symptoms. Learn about more ways hormones can become disrupted here.
Further, living in the modern world brings a constant exposure to environmental toxins such as plastics and other chemicals; those that have hormonal effects are known as endocrine disrupting chemicals (EDCs). EDCs such as bisphenol A (BPA) found in the lining of tins can actually increase oestrogen and change the way it works in the body. Read more about this here.
Be Proactive About Keeping Oestrogen in Balance
If your pain, PMS or hormonal symptoms may be caused by too much oestrogen, then it’s time to take back control. There are many positive steps you can take towards rebalancing your hormones.
Many herbs and nutrients can be extremely beneficial in reigning in out-of-control hormones. Isoflavones from soy are used to support women’s healthy oestrogen levels by modulating oestrogen receptors (the binding sites on the cells).7 This means that soy can effectively instruct cells to promote the healthy actions of oestrogen and turn down the dial down on the more negative impacts. Read more about soy in this article. Other natural medicines such as magnesium, broccoli, rosemary, and BCM-95™ Turmeric all have positive effects on supporting healthy oestrogen metabolism, helping to restore a state of balance.
There are also some simple strategies you can adopt on a daily basis to place you on the path of healthy oestrogen balance. Follow the healthy hormone dietary and lifestyle tips in Figure 3 below. Other suggestions include not microwaving food in plastic containers, and swapping your plastic drinking bottles for glass or stainless steel – this can help reduce the impact of EDCs exposure. For more simple tips to detox your environment check out this blog.

Figure 3: Healthy Hormone Diet and Lifestyle Tips.
By gradually changing your habits you can reduce exposure to harmful EDCs, improve your oestrogen metabolism, and maintain the beneficial effects that the beautiful hormone called oestrogen may bring. If you would like more support in improving hormonal harmony and freeing yourself from the symptoms of oestrogen imbalance, speak to your local natural healthcare Practitioner today.
References
1. Cutter WJ, Norbury R, Murphy DGM. Oestrogen, brain function, and neuropsychiatric disorders. J Neurol Neurosurg Psychiatry.2003 Jul;74(7):837-840.
2. Shah MG, Maibach HI. Estrogen and skin. An overview. Am J Clin Dermatol. 2001;2(3):143-50. PMID: 11705091
3. Greenspan FS, Gardner DG. Basic and clinical endocrinology. 6th ed. Sydney, Australia: Lange Medical Books/McGraw-Hill; 2001. p. 575-602.
4. Ferrero S, Remorgida V, Maganza C, Venturini PL, Salvatore S, Papaleo E, et al. Aromatase and endometriosis: estrogens play a role. Ann N Y Acad Sci. 2014 May;1317:17-23. doi: 10.1111/nyas.12411
5. Bulun SE, Lin Z, Imir G, Amin S, Demura M, Yilmaz B, et al. Regulation of aromatase expression in estrogen-responsive breast and uterine disease: from bench to treatment. Pharmacol Rev. 2005 Sep;57(3):359-83. doi: 10.1124/pr.57.3.6.
6. Chetrite GS, Cortes-Prieto J, Philippe JC, Wright F, Pasqualini JR. Comparison of estrogen concentrations, estrone sulfatase and aromatase activities in normal, and in cancerous, human breast tissues. J Steroid Biochem Mol Biol. 2000 Jan-Feb;72(1-2):23-7. PMID: 10731634.
7. Kuiper GG, Lemmen JG, Carlsson B, Corton JC, Safe SH, van der Saag PT, et al. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology. 1998 Oct;139(10):4252-4263.
We all have those days…😉
So what is MANOPAUSE?

Testosterone levels begin to rise in puberty, reach their maximum in a man’s early twenties, and gradually begin to decline from then on. From about the age of 30 men tend to lose about 1% of their testosterone each year – this is normal.
However, as average peak testosterone levels in men have dropped by approximately 20% over the past 40 years, more and more men are experiencing the negative effects of lower testosterone as they age.
Everyone has heard of menopause, the stage of life whereby a women’s sex hormone levels begin to decline. The use of the term ‘manopause’ (or andropause) however is becoming increasingly common, used to describe the correlating condition in ageing males. Some cardinal symptoms of ‘manopause’ include:
- A reduction of sexual thoughts or desire;
- Trouble achieving or maintaining an erection;
- Lower energy levels;
- Mood changes;
- Loss of muscle mass and bone density;
- Reduction in cognitive function; and/or
- Mood disturbances.
Under normal circumstances, testosterone production is tightly regulated within the body. Initially, signalling hormones are produced by the brain, and travel to the testicles to stimulate testosterone production. As testosterone production increases, the brain receives the message there is enough testosterone within the body and stops telling the testicles to produce it. Once levels start to fall, the brain then produces more signalling hormones to stimulate the production of testosterone. This feedback system is what keeps levels of testosterone optimal and the male body healthy.

However, there are a number of factors that can interfere with normal testosterone production and utilisation:
- Once produced, testosterone can be converted into other hormones by enzymes, the two most important called aromatase and 5-alpha reductase. Increased activity of these enzymes can contribute to symptoms of ‘manopause’ by reducing levels of available testosterone.
- Aromatase is found particularly in fat tissues, and it’s activity is up-regulated by inflammation. Aromatase actually converts testosterone to oestrogen, meaning excess weight and inflammation can cause a reduction in testosterone and an increase in oestrogen (which we don’t want too much of in men).
- 5-alpha reductase converts testosterone to a very active form of testosterone called dihydrotestosterone (DHT). While DHT promotes growth in skeletal muscle, too much can also cause the prostate to enlarge (a condition known as benign prostate hyperplasia) and trigger hair loss in hereditary male pattern baldness. Unfortunately, this activity of DHT is largely determined by genetics.
- Nutritional deficiencies can also inhibit the production of testosterone.
Adequate intake of protein, essential fatty acids, zinc and selenium is crucial to provide the necessary building blocks for testosterone production.
- Chronic stress can also reduce testosterone production in a number of ways.
- The ‘ingredients’ (or structural components) required for testosterone production are also used to produce the stress hormone cortisol. Excess production of stress hormones on a long-term basis reduces the amount of ingredients available for testosterone production.
- Cortisol levels can also directly inhibit testosterone production in the testes, as well as the production of the testosterone signalling hormones in the brain.

While there may be complex processes reducing testosterone production, the good news is that many of these can be addressed by simple diet and lifestyle interventions:
- Eat a balanced diet rich in antioxidants, minerals and essential fatty acids to provide all of the building blocks for healthy testosterone production.
- Maintain a healthy body composition, keeping body fat levels down to reduce the conversion of testosterone to oestrogen by aromatase.
- Tackle inflammation by addressing lifestyle factors such as sugar and alcohol consumption, further reducing aromatase activity.
- Learn to manage stress effectively, and ensure good quality sleep to regulate cortisol production, which is crucial for maintaining healthy testosterone levels as you age.
Lastly, there are a number of herbs that have been shown to support testosterone levels and male reproductive health. For example, Tribulus terrestris or ‘tribulus’ has been shown to enhance testosterone in animal studies, and has a long history of use in traditional Ayurvedic medicine to support virility and sexual desire. Similarly, the intriguingly named ‘horny goat weed’ (whose correct Latin name is Epimedium sagittatum) is a traditional male tonic indicated for impotence, as an aphrodisiac, and to enhance sperm production. For optimal results, these herbs should be combined with supplementary zinc (if required), along with the diet and lifestyle strategies above.
Even if the more superficial aspects of testosterone deficiency are not of concern, the role that testosterone plays in wellness and ageing means that all men who wish to live a long and healthy life should be looking to support their testosterone levels in a natural, holistic manner. So if you are feeling fatigued or cranky, your mojo isn’t wasn’t it used to be or you notice that you are losing muscle mass, it could mean that you have low testosterone. If so, work with a qualified healthcare Practitioner to uncover and address the underlying causes, such as those discussed above, to ensure your quality of life now and into old age.

 Is What You Heard About Turmeric True?
Is What You Heard About Turmeric True? 

