Microbiome 101
‘Microbiome’ is a hot topic right now for anyone interested in health; but you may be wondering what exactly it is? You’ve potentially heard about the good bacteria living within your digestive system, and may have even thought about taking a probiotic to support them. Well it’s this internal community – actually encompassing a massive 38 trillion microbes (not just bacteria) – that are collectively referred to as your commensal microbiome. When healthy and balanced, your microbiome has wide-reaching health effects, such as synthesising important vitamins you need; helping to modulate and boost your immune system; assisting with waste elimination (therefore supporting healthy bowel function); and even influencing your mood.1
However, your diet and lifestyle choices can negatively impact the health of your microbiome; resulting in a reduction in both the numbers and/or diversity of the organisms within your gut. Disruption to your internal microbial community can then create an environment where pathogenic (disease causing) organisms have the opportunity to grow and prosper. This state of imbalance is termed ‘dysbiosis’, and can lead to a plethora of negative health effects, including digestive complaints, nutrient deficiencies, or maybe a compromised immune system (which can lead to allergies and/or frequent illness) – these are all common outcomes when the microbiome becomes imbalanced.
The following are five of the most common diet and lifestyle factors that may negatively impact the health of your microbiome, along with some tips to help you re-establish a healthy and thriving microbial community once more.
Five ways you can upset your microbiome:
- Eating a low fibre diet: as your gut microbes rely on the fibre in your food for fuel, a low fibre diet leads to a reduction in the diversity of your microbiome.
Interestingly, evidence now shows those who consume more than 30 different types of plants/vegetables each week have a much more diverse microbiome compared to those who consume 10 or fewer types of plants weekly.2
- Alcohol intake: the consumption of alcohol can result in dysbiotic changes in your intestinal microbiome, and also triggers gastrointestinal inflammation.3 If you’re consuming more than one standard drink per day, your microbiome’s probably keen for you to abstain a bit more often!
- Unmanaged stress: when you are stressed, the release of the stress hormone cortisol, and adrenaline sensitise your body to inflammation, including gut inflammation.4 This disrupts the gut environment, compromising the conditions your beneficial microbes need to flourish.
- Leading a sedentary lifestyle: lack of exercise has also been linked to reduced microbial diversity in the gut – another reason to get moving!
- Antibiotic use: a round of antibiotics does lead to some loss of core commensal organisms (antibiotics are supposed to kill off bacteria however in this instance the good stuff goes too). This leaves the gut susceptible to microbiome imbalances and dysfunction. Due to this disruption, up to 10% of people experience gastrointestinal side effects5 from antibiotic use, referred to as antibiotic-associated diarrhoea (AAD).6,7
Do any of these situations apply to you? Fortunately, there are a few things you can do to support your microbiome and help correct any imbalance.

Fighting, Fixing and Fuelling
Addressing the five diet and lifestyle factors listed above is important for improving the health and diversity of your microbiome. Managing your stress levels, utilising antibiotics only when specifically needed (and taking stain-specific probiotic to restore your microbiome if you do), moderating your alcohol intake, and regularly exercising will all have your microbiome singing your praises! Additionally, and perhaps most importantly, consuming a diet rich in plant based fibres will provide ample fuel for your beneficial organisms to flourish. See Table 1 below for ideas on foods your microbiome loves.
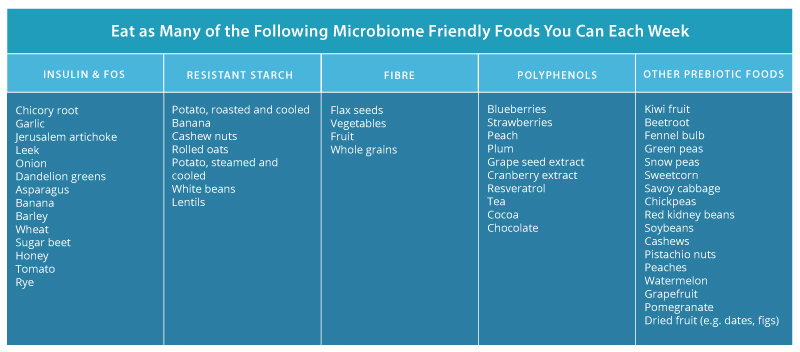
Table 1: Foods That Feed Your Microbiome
Nevertheless, there are situations where pathogenic organisms have the opportunity to establish within your gut and create dysbiosis, requiring specific natural formulations to address it. In this instance, antimicrobial herbal medicines can be employed, including pomegranate (Punica granatum),8 nigella (Nigella sativa),9 and myrrh (Commiphora myrrha).10, 11 These herbs work to eliminate unwanted organisms within the gut, and have even shown to be as effective as their pharmaceutical counterparts in helping to reduce pathogenic populations in scientific research.
However, while eliminating pathogenic species can begin to address an imbalanced microbiome, this is only one part of the puzzle. You also need to focus on regenerating and rebuilding the diversity of your commensal microbiome, which can be achieved with specific probiotic strains such as:
-
- Lactobacillus rhamnosus (LGG®): one of the most studied probiotic stains in the world, research shows LGG®administration to promote the growth and function of key core commensal bacteria.
- Saccharomyces cerevisiae (boulardii) (SB): multiple investigations have shown that boulardii reduces antibiotic-associated loss of bacteria, whilst also supporting the rapid restoration of the microbiome after antibiotic use.12
- Lactobacillus acidophilus (NCFM®)13 and Bifidobacterium animalis lactis (Bi-07): are two strains also highly indicated to protect and support a healthy microbiome.14

So whilst there are factors that can upset your microbiome, be assured there is also a multitude of natural medicines, diet and lifestyle options you can harness to encourage it’s health too, and hence the wellbeing of your whole body. Many of these tips are under your control, but if you feel you need some extra help and support with antimicrobial herbs and/or strain-specific probiotics talk to your healthcare Practitioner about a tailored microbiome-restoring treatment plan to suit your needs. Your beneficial bugs will thank you for it!
References
1. D’Argenio S. The role of the gut microbiome in the healthy adult status. Clinica Chimica Acta. 2015;451(Part A):97-102.
2. Buschman H, Bright D. Big Data from World’s Largest Citizen Science Microbiome Project Serves Food for Thought. [Internet]. San Diego (CA): UC San Diego School of Medicine. 2018 [cited 2018 July 05]. Available from: https://health.ucsd.edu/news/releases/Pages/2018-05-15-big-data-from-worlds-largest-citizen-science-microbiome-project-serves-food-for-thought.aspx
3. Engen PA, Green SJ, Voiqt RM, Forsyth CB, Keshavarzian A. The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota. Alcohol Res. 2015;37(2):223-36.
4. Guilliams TG. The role of stress and the HPA axis in chronic disease management. Point Institute, Stevens point (WI). 2015;80.
5. NPS Medicinewise. What are the side effects of antibiotics? [Internet]. Sydney NSW: NPS Medicinewise; 2012 [updated 2017 Mar; cited 2018 July 05]. Available from: http://www.nps.org.au/medicines/infections-and-infestations/antibiotics/for-individuals/side-effects-of-antibiotics.
6. Eloe-Fedrosh E, Brady A ,Crabtree J, Drabek E, Ma B, Mahurkar A, et al. Functional dynamics of the gut microbiome in elderly people during probiotic consumption. M Bio. 2015 Apr 14;16(2):e00231-15.
7. McFarland L. Use of probiotics to correct dysbiosis of normal microbiota following disease or disruptive events: a systematic review. BMJ Open. 2014 Aug 25;4(8):e005047.
8. Abdel-Haffez E, Ahmed A, Abdellatif M, Kamal A, Toni N. The efficacy of pomegranate (Punica granatum) peel extract on experimentally infected rats with blastocystis spp. J Infect Dis Preve Med. 2016;4(1):1-6.
9. Salem EM, Yar T, Bamosa AO, Al-Quorain A, Yasawy MI, Alsulaiman RM, et al. Comparative study of Nigella sativa and triple therapy in eradication of Helicobacter pylori in patients with non-ulcer dyspepsia. Saudi J Gastroenterol. 2010 Jul;16(3):207.
10. Fathy FM. Effect of mirazid (Commiphora molmol) on experimental giardiasis. J Egypt Soc Parasitol. 2011 Apr;41(1):155-77.
11. Basyoni MM, El-Sabaa AA. Therapeutic potential of myrrh and ivermectin against experimental Trichinella spiralis infection in mice. Korean J Parasitol. 2013 Jun;51(3):297-304. doi: 10.3347/kjp.2013.51.3.297.
12. Moré M, Swidsinski A. Saccharomyces boulardii CNCM 1-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis – a review. Clinical and Experimental Gastroenterology. 2015;8:237-55.
13. Anderson JM, Barrangou R, Hachem MA, Lahtinen SJ, Goh YJ, Svensson B, et al. Transcriptional analysis of prebiotic uptake and catabolism by Lactobacillus acidophilus NCFM. PLos ONE. 2012;7(9):e44409.
14. Mäkeläinen H, Saarinen M, Stowell J, Rautonen N, Ouwehand AC. Xylo-oligosaccharides and lactitol promote the growth of Bifidobacterium lactis and Lactobacillus species in pure cultures. Benef Microbes. 2010 Jun;1(2):139-48