How can you prepare for the FLU SEASON?🤧
Are your prepared for the cold and flu season? You might be feeling fine right now but even the healthiest of us can succumb to a stray virus at this time of year, resulting in days off work and…even worse…keeping you indoors and missing out on the things you love to do. Fortunately there are some surprisingly helpful little microbes you may not know about that are your winter allies – capable of helping your immune system search out viral invaders and reducing the chance of an infection taking hold. These little microbes are probiotics.
Knowing the Strain is the Key to Choosing the Right Probiotic
It’s become common knowledge that probiotics can help with gut function and digestive health – that’s perhaps what they are best known for. What you may not know though is your gut contains approximately 70% of your body’s immune system,[1] and knowing that, you may not be so surprised to hear that certain probiotics can influence the activity of your immune cells. So how do you know which ones these are?
First you need to understand that there are many different beneficial probiotics available and each one has a different role to play in human health.
As such, the way to make sure you are using the right probiotic for your needs is to check the specific genus, species and strain (see Figure 1) has been used in human clinical trials for the condition you want to use it for – in this case reducing the likelihood of you contracting a cold or flu – because not every probiotic would be indicated for this condition.
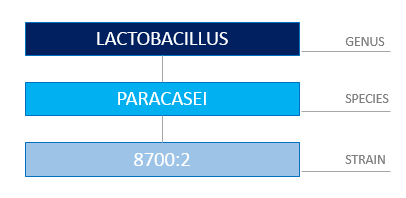
Figure 1: Correctly Identifying a Probiotic Requires You to Know the Genus, Species and Strain.
You may be wondering how a probiotic can enhance immune system function. To begin with, the microbial life living within your gastrointestinal tract (known as your gut microbiota) play an important role in maintaining the lining of your gut, which itself forms an intestinal defense barrier – so that’s one of the ways many probiotics can help – by supporting the health of the microbiota already residing within you.
However, certain probiotic strains have the ability to actually communicate directly with your immune cells, thus influencing and improving the immune response.[2]
Two of these probiotic strains are Lactobacillus rhamnosus (LGG®)[3] and Lactobacillus paracasei 8700:2,[4] both of which increase the activity of immune cells called natural killer (NK) cells – who, as their name suggest, actually target and kill virally infected cells – exactly what you want to tackle a cold or flu.
In addition, Lactobacillus paracasei 8700:2 and Lactobacillus plantarum HEAL 9 are two specific strains that stimulate other white blood cells (called ‘macrophages’) to secrete an important chemical signal that alerts your immune system to mount an antiviral immune response.[5],[6] Lastly, Lactobacillus plantarum HEAL 9, Lactobacillus paracasei 8700:2 and LGG® all have the capacity to trigger a natural chemical messenger inside your body called interleukin-10, which is a key anti-inflammatory and immune-regulating signal.[7],[8] Now that may all seem quite technical but what it helps demonstrate is that, used together, these three probiotic strains play a valuable role in supporting healthy immune system function.
Where’s the Evidence?
This isn’t all just theory; the ability of Lactobacillus plantarum HEAL 9 and Lactobacillus paracasei 8700:2 to improve immune function has been demonstrated in a randomised, controlled trial. Two hundred and seventy-two healthy adults were given 500 million CFU* each of Lactobacillus plantarum HEAL 9 and Lactobacillus paracasei 8700:2, or placebo, for 12 weeks. Those in the treatment group experienced fewer incidences of the common cold, with significantly reduced duration and symptom severity when infection did occur.[9] A combination of these two specific strains has also been shown to reduce symptom severity and duration of the common cold in subjects who are prone to recurrent infections.[10]
What this all tells you is these probiotic strains have actually been tested in real situations and shown to be helpful in not only preventing colds and flus but, when someone got sick, they reduced the numbers of sick days taken – essentially the people taking these probiotic strains recovered faster.
Prevention is Better Than Cure
Don’t wait until you get sick this year, or assume there is nothing you can do about it. If you have a history of frequent colds and flus (or maybe you were one of the people who succumbed to that debilitating flu that did the rounds in Australia in 2017), don’t just pop to the pharmacy and grab any probiotic; be strategic and speak to your Naturopath or other healthcare Practitioner first, and ask them how best to improve your immune surveillance with probiotic strains proven to enhance immunity.
You can also help support yourself by managing your stress levels (stress depletes your immune system), eating plenty of colourful vegetables and fruits, nuts and seeds (to improve your overall nutritional status – more on that in an upcoming blog post), and look after your gut health – remember, the gut is where much of your immune system is located. Take practical steps now to reduce the likelihood of you getting sick this winter, and enjoy the colder months healthy and well.
* CFU means ‘colony forming units’ and is what tells you these were live bacteria. Either CFU or ‘live bacteria’ are important things to look for on a probiotic label so you know the product contains viable organisms. Also – the specific strain must be listed on the label – if it is missing then don’t use the probiotic…you don’t know what it is!
References
[1] Gill HS. Probiotics to enhance anti-infective defences in the gastrointestinal tract. Best Practice and Research Clinical Gastroenterology. 2003;17(5):755-773.
[2] Lebeer S, Vanderleyden J, De Keersmaecker SC. Host interactions of probiotic bacterial surface molecules: comparison with commensals and pathogens. Nature Reviews Microbiology. 2010;8:171-184.
[3] Harata G, He F, Hiruta N, Kawase M, Kubota A, Hiramatsu M, et al. Intranasal administration of Lactobacillus rhamnosus GG protects mice from H1N1 influenza virus infection by regulating respiratory immune responses. Lett Appl Microbiol. 2010;50:597-602.
[4] Rask C, Adlerberth I, Berggren A, Ahren IL, Wold AE. Differential effect on cell-mediated immunity in human volunteers after intake of different lactobacilli. Clinical and Experimental Immunology. 2013;172(2):321-32.
[5] Rask C, Adlerberth I, Berggren A, Ahren IL, Wold AE. Differential effect on cell-mediated immunity in human volunteers after intake of different lactobacilli. Clinical and Experimental Immunology 2013;172(2):321-32.
[6] Leonard P, Sur S. Interleukin-12: potential role in asthma therapy. BioDrugs. 2003;17(1):1-7.
[7] Lavasani S, Dzhambazov B, Nouri M, Kak F, Buske S, Molin G, et al. A novel probiotic mixture exerts a therapeutic effect on experimental autoimmune encephalomyelitis mediated by IL-10 producing regulatory T cells. PLoS ONE. 2010;5(2):e9009.
[8] Feleszko W, Jaworska J, Rha RD, Steinhausen S, Avagyan A, Jaudszus A, et al. Probiotic-induced suppression of allergic sensitization and airway inflammation is associated with an increase of Tregulatory-dependent mechanisms in a murine model of asthma. Clin Exp Allergy. 2007;37(4):498-505.
[9] Berggren A, Lazou A, Larsson N, Onning G. Randomised, double-blind and placebo-controlled study using new probiotic lactobacilli for strengthening the body immune defence against viral infections. Eur J Nutr. 2011;50(3):203-210.
[10] Busch R, Gruenwald J, Dudek S. Randomised, double blind and placebo controlled study using a combination of two probiotic lactobacilli to alleviate symptoms and frequency of common cold. Food and Nutrition Sciences. 2013;4:13-20.
It’s not until your unwell🤒🤧🤕, that you realise…🍃
Did YOU KNOW?🤔🥂🥦🤦♀️🏃♀️💊
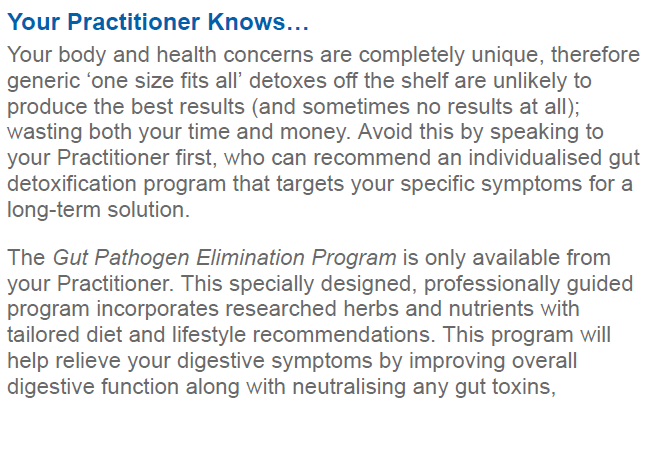
Microbiome 101
‘Microbiome’ is a hot topic right now for anyone interested in health; but you may be wondering what exactly it is? You’ve potentially heard about the good bacteria living within your digestive system, and may have even thought about taking a probiotic to support them. Well it’s this internal community – actually encompassing a massive 38 trillion microbes (not just bacteria) – that are collectively referred to as your commensal microbiome. When healthy and balanced, your microbiome has wide-reaching health effects, such as synthesising important vitamins you need; helping to modulate and boost your immune system; assisting with waste elimination (therefore supporting healthy bowel function); and even influencing your mood.1
However, your diet and lifestyle choices can negatively impact the health of your microbiome; resulting in a reduction in both the numbers and/or diversity of the organisms within your gut. Disruption to your internal microbial community can then create an environment where pathogenic (disease causing) organisms have the opportunity to grow and prosper. This state of imbalance is termed ‘dysbiosis’, and can lead to a plethora of negative health effects, including digestive complaints, nutrient deficiencies, or maybe a compromised immune system (which can lead to allergies and/or frequent illness) – these are all common outcomes when the microbiome becomes imbalanced.
The following are five of the most common diet and lifestyle factors that may negatively impact the health of your microbiome, along with some tips to help you re-establish a healthy and thriving microbial community once more.
Five ways you can upset your microbiome:
- Eating a low fibre diet: as your gut microbes rely on the fibre in your food for fuel, a low fibre diet leads to a reduction in the diversity of your microbiome.
Interestingly, evidence now shows those who consume more than 30 different types of plants/vegetables each week have a much more diverse microbiome compared to those who consume 10 or fewer types of plants weekly.2
- Alcohol intake: the consumption of alcohol can result in dysbiotic changes in your intestinal microbiome, and also triggers gastrointestinal inflammation.3 If you’re consuming more than one standard drink per day, your microbiome’s probably keen for you to abstain a bit more often!
- Unmanaged stress: when you are stressed, the release of the stress hormone cortisol, and adrenaline sensitise your body to inflammation, including gut inflammation.4 This disrupts the gut environment, compromising the conditions your beneficial microbes need to flourish.
- Leading a sedentary lifestyle: lack of exercise has also been linked to reduced microbial diversity in the gut – another reason to get moving!
- Antibiotic use: a round of antibiotics does lead to some loss of core commensal organisms (antibiotics are supposed to kill off bacteria however in this instance the good stuff goes too). This leaves the gut susceptible to microbiome imbalances and dysfunction. Due to this disruption, up to 10% of people experience gastrointestinal side effects5 from antibiotic use, referred to as antibiotic-associated diarrhoea (AAD).6,7
Do any of these situations apply to you? Fortunately, there are a few things you can do to support your microbiome and help correct any imbalance.

Fighting, Fixing and Fuelling
Addressing the five diet and lifestyle factors listed above is important for improving the health and diversity of your microbiome. Managing your stress levels, utilising antibiotics only when specifically needed (and taking stain-specific probiotic to restore your microbiome if you do), moderating your alcohol intake, and regularly exercising will all have your microbiome singing your praises! Additionally, and perhaps most importantly, consuming a diet rich in plant based fibres will provide ample fuel for your beneficial organisms to flourish. See Table 1 below for ideas on foods your microbiome loves.
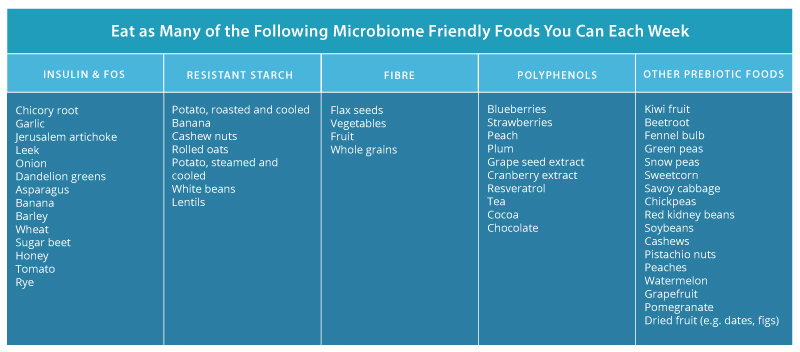
Table 1: Foods That Feed Your Microbiome
Nevertheless, there are situations where pathogenic organisms have the opportunity to establish within your gut and create dysbiosis, requiring specific natural formulations to address it. In this instance, antimicrobial herbal medicines can be employed, including pomegranate (Punica granatum),8 nigella (Nigella sativa),9 and myrrh (Commiphora myrrha).10, 11 These herbs work to eliminate unwanted organisms within the gut, and have even shown to be as effective as their pharmaceutical counterparts in helping to reduce pathogenic populations in scientific research.
However, while eliminating pathogenic species can begin to address an imbalanced microbiome, this is only one part of the puzzle. You also need to focus on regenerating and rebuilding the diversity of your commensal microbiome, which can be achieved with specific probiotic strains such as:
-
- Lactobacillus rhamnosus (LGG®): one of the most studied probiotic stains in the world, research shows LGG®administration to promote the growth and function of key core commensal bacteria.
- Saccharomyces cerevisiae (boulardii) (SB): multiple investigations have shown that boulardii reduces antibiotic-associated loss of bacteria, whilst also supporting the rapid restoration of the microbiome after antibiotic use.12
- Lactobacillus acidophilus (NCFM®)13 and Bifidobacterium animalis lactis (Bi-07): are two strains also highly indicated to protect and support a healthy microbiome.14

So whilst there are factors that can upset your microbiome, be assured there is also a multitude of natural medicines, diet and lifestyle options you can harness to encourage it’s health too, and hence the wellbeing of your whole body. Many of these tips are under your control, but if you feel you need some extra help and support with antimicrobial herbs and/or strain-specific probiotics talk to your healthcare Practitioner about a tailored microbiome-restoring treatment plan to suit your needs. Your beneficial bugs will thank you for it!
References
1. D’Argenio S. The role of the gut microbiome in the healthy adult status. Clinica Chimica Acta. 2015;451(Part A):97-102.
2. Buschman H, Bright D. Big Data from World’s Largest Citizen Science Microbiome Project Serves Food for Thought. [Internet]. San Diego (CA): UC San Diego School of Medicine. 2018 [cited 2018 July 05]. Available from: https://health.ucsd.edu/news/releases/Pages/2018-05-15-big-data-from-worlds-largest-citizen-science-microbiome-project-serves-food-for-thought.aspx
3. Engen PA, Green SJ, Voiqt RM, Forsyth CB, Keshavarzian A. The Gastrointestinal Microbiome: Alcohol Effects on the Composition of Intestinal Microbiota. Alcohol Res. 2015;37(2):223-36.
4. Guilliams TG. The role of stress and the HPA axis in chronic disease management. Point Institute, Stevens point (WI). 2015;80.
5. NPS Medicinewise. What are the side effects of antibiotics? [Internet]. Sydney NSW: NPS Medicinewise; 2012 [updated 2017 Mar; cited 2018 July 05]. Available from: http://www.nps.org.au/medicines/infections-and-infestations/antibiotics/for-individuals/side-effects-of-antibiotics.
6. Eloe-Fedrosh E, Brady A ,Crabtree J, Drabek E, Ma B, Mahurkar A, et al. Functional dynamics of the gut microbiome in elderly people during probiotic consumption. M Bio. 2015 Apr 14;16(2):e00231-15.
7. McFarland L. Use of probiotics to correct dysbiosis of normal microbiota following disease or disruptive events: a systematic review. BMJ Open. 2014 Aug 25;4(8):e005047.
8. Abdel-Haffez E, Ahmed A, Abdellatif M, Kamal A, Toni N. The efficacy of pomegranate (Punica granatum) peel extract on experimentally infected rats with blastocystis spp. J Infect Dis Preve Med. 2016;4(1):1-6.
9. Salem EM, Yar T, Bamosa AO, Al-Quorain A, Yasawy MI, Alsulaiman RM, et al. Comparative study of Nigella sativa and triple therapy in eradication of Helicobacter pylori in patients with non-ulcer dyspepsia. Saudi J Gastroenterol. 2010 Jul;16(3):207.
10. Fathy FM. Effect of mirazid (Commiphora molmol) on experimental giardiasis. J Egypt Soc Parasitol. 2011 Apr;41(1):155-77.
11. Basyoni MM, El-Sabaa AA. Therapeutic potential of myrrh and ivermectin against experimental Trichinella spiralis infection in mice. Korean J Parasitol. 2013 Jun;51(3):297-304. doi: 10.3347/kjp.2013.51.3.297.
12. Moré M, Swidsinski A. Saccharomyces boulardii CNCM 1-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis – a review. Clinical and Experimental Gastroenterology. 2015;8:237-55.
13. Anderson JM, Barrangou R, Hachem MA, Lahtinen SJ, Goh YJ, Svensson B, et al. Transcriptional analysis of prebiotic uptake and catabolism by Lactobacillus acidophilus NCFM. PLos ONE. 2012;7(9):e44409.
14. Mäkeläinen H, Saarinen M, Stowell J, Rautonen N, Ouwehand AC. Xylo-oligosaccharides and lactitol promote the growth of Bifidobacterium lactis and Lactobacillus species in pure cultures. Benef Microbes. 2010 Jun;1(2):139-48
How you you boost your IMMUNE SYSTEM?
Are you sick of always being sick? Do you ever feel like a sitting duck waiting to be taken down by the latest pathogen doing the office rounds? Or perhaps you’ve tried to remember when the last time was you got through a whole winter season without several bouts of illness? If either of these thoughts have crossed your mind then you need to be getting some immune ‘R n R’; that is – better immune resistance and resilience.
An immune system lacking either can make you susceptible to recurrent bouts of illness. For example, if your immune system is struggling to reclaim it’s vitality after one bout of illness, then you will be susceptible to the next lot of bugs doing the rounds and hence you come down with a secondary infection. This can create the illusion that a particularly horrible virus must be on your tail. However, in this scenario, your dragging symptoms may not be entirely caused by the power of the pathogen in your system, but due to a weakened immune response, unable to resist the invader. As such, that re-appearing tickly throat or glands swelling up again can be a tell-tale sign of your immune system losing ground.
Restoring Resilience Starts With Lifestyle
No one is exempt from the many factors that can hinder your immune system – stress, lack of sleep and the inevitable balancing act of modern day life – all of which deplete our energy, hindering our degree of immune resistance and resilience. Interestingly, even your thoughts can influence your recovery time from an infection,[1] highlighting the importance of developing a healthy mind-set. Nourishing habits to support mental wellbeing include making time to promote relaxation such as meditation, as well as light exercise; both particularly useful in reducing the immunosuppressive effects of an overactive stress response,[2] which can simply be due to a busy life, or actual stressful events. On the other hand, ‘coping’ strategies such as consuming alcohol [3] and smoking [4] do the opposite – increasing your risk of infection and disease. This goes to show that positive lifestyle choices can support your road recovery, and help you break the cycle of recurrent infection.
Eating Your Way to Recovery…and Resilience
Most people are aware that eating a good diet pays dividends, but how well do you actually nourish your body during those times you feel most exhausted and fragile? You’ve potentially heard about the ‘flight and fight’ response, but did you know that the opposite of this phrase is ‘rest and digest’? Real rest is achieved by taking enough time to fully recover when you do become unwell, and acknowledging how you can best meet your needs by ensuring you are resting enough at busy times. Digest refers to the process of assimilating the nutrients from your diet, so healthy digestion is crucial to good health…and good immune function. If you have any digestive issues – speak to your healthcare Practitioner who can help investigate what’s going on.
Some foods offer significant advantages when it comes to a robust immune system. Firstly, warming foods such as crockpot stews and soups save your body time and effort breaking down raw or dense ingredients, leaving you more energy for healing if you become unwell. Secondly, consuming protein-rich foods such as eggs, legumes, nuts, and seeds ensure you have adequate nutritional resources to create new armies of immune cells, to orchestrate the destruction of a pathogenic bugs when you do come into contact with them. Finally, nutrients which are tricky to obtain, either due to low soil levels or dietary restriction, should be bolstered through supplementation where necessary – your Practitioner can help you assess if these are required. Key natural medicines, if you are lacking, ensures your body is adequately supported by the essential nutrients required to promote an active immune response and facilitate better resilience.
Natural Ingredients Have Your Back
You’ve probably heard there are certain probiotics, herbs and nutrients used to promote good health, but did you know that many of these natural ingredients actually work with your own immune system rather than just being a ‘Band-Aid’ for symptoms? For instance, nutrients such as zinc and vitamin D provide protection against infectious agents by reinforcing the strength of the immune barrier between you and the outside world,[5],[6] namely your gut lining. Furthermore, the immunostimulatory constituents (called polysaccharides) found in certain medicinal mushrooms including Trametes versicolor (coriolus) and Ganoderma lucidum (reishi), as well as in the herb Astragalus membranaceus (astragalus) activate several of the internal agents you need for healthy immune system surveillance and resilience (see Figure 1).
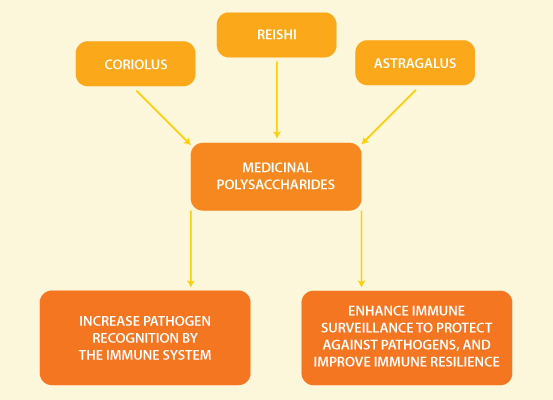
Figure 1: The Immunostimulatory Effects of Medicinal Polysaccharides.
These actions include increasing what’s known as secretory immunoglobulin A on the mucosal surface lining your gut, [7] as well as promoting the activity of immune cells called macrophages (which translates to ‘large eaters’ giving you a picture of what they do to pathogens!) and natural killer cells,[8] whose task is to destroy infection-causing invaders.
Taking a natural medicine approach to your health offers you so many proactive ways to improve your immune resilience in order to prevent ongoing episodes of immune dysfunction…namely illness! By addressing the underlying causes of why you keep getting sick in a holistic way, you can re-write your immune story into one which features resistance and resilience as hero’s and focus instead on enjoying all the things in life you love.
References
[1] Van Schrojenstein Lantman M, Mackus M, Otten LS, de Kruijff D, van de Loo AJ, Kraneveld AD, et al. Mental resilience, perceived immune functioning, and health. J Multidiscip Healthc. 2017 Mar 21;10:107-112. doi: 10.2147/JMDH.S130432.
[2] Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004 May 1;29(4):448-74.
[3] Sarkar D, Jung MK, Wang HJ. Alcohol and the immune system. Alcohol research: current reviews. 2015;37(2):153.
[4] Huttunen R, Heikkinen T, Syrjänen J. Smoking and the outcome of infection. Journal of internal medicine. 2011 Mar 1;269(3):258-69.
[5] Assa A, Vong L, Pinnell LJ, Avitzur N, Johnson-Henry KC, Sherman PM. Vitamin D deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J Infect Dis. 2014 Apr 21;210(8):1296-305.
[6] Zhong W, McClain CJ, Cave M, Kang YJ, Zhou Z. The role of zinc deficiency in alcohol-induced intestinal barrier dysfunction. Am J Physiol Gastrointest Liver Physiol. 2010 Feb 18;298(5):G625-33.
[7] He X, Niu X, Li J, Xu S, Lu A. Immunomodulatory activities of five clinically used Chinese herbal polysaccharides. J Experimental Integrative Med. 2012:2(1):15-27.
So TRUE!💞
Ready for a myth bust?
All the Noise About Soy
Myth #1: Soy is a goitrogen.
Fact: Goitrogens are substances that disrupt the production of thyroid hormone by interfering with the uptake of iodine into the thyroid gland. Soy has previously been classified as a goitrogen; however, this was based primarily on observations yielded from in vitro and animal studies,1 which in this instance offer limited relevance to humans due to differing metabolism between human and animals with regards to soy.2 That said, in situations of inadequate dietary iodine intakes, thyroid symptoms caused by this lack may be amplified by simultaneously high intakes of soy.3 Nevertheless, a comprehensive review of 14 human clinical studies provided little evidence that soy exerts anti-thyroid effects in healthy subjects,4 which is further supported by the European Food Safety Authority (EFSA).5
In summary, human evidence supports the safe consumption of dietary soy6,7 alongside adequate iodine intake.8
Myth #2: All soy is genetically modified.
Fact: In the past decade, there has been a surge in the production of genetically modified (GM) crops, with soy representing one of those most commonly affected. Genetically modified organisms (GMO) are those whose genetic material has been altered using genetic engineering techniques designed to produce specific traits. It is true that without sufficient data we can’t predict the effects of modified proteins, so selecting non-GMO soy products avoids unknown risks. As such, non-GMO sources of soy are available, and consuming it in this natural and unadulterated wholefood form is always advised for maximal health benefits.

The Humble Soybean Manifests in Many Dietary Ways.
Myth #3: You should only eat soy if it’s fermented.
Fact: In early China, soy was traditionally cooked like a grain. Processing of this legume then evolved across different regions of Asia to become a variety of modes like those illustrated in Figure 1. This included fermenting (to create tempeh, miso and natto), sprouting, grinding to make a ‘milk,’ and the pressing of unfermented bean curd to create tofu. Fermentation is especially favored in Korea and Japan for producing strong flavours, however doing so is not the golden rule for soy consumption. Similar to other legumes, simply softening soybeans with moisture and heat (e.g. boiling) causes the hardy components within the bean to denature. This allows the nutrients to then become bioavailable and absorbable, and therefore allow us to attain the benefits from consuming them.
In summary, soy has not always traditionally been fermented, and it is perfectly safe and appropriate to consume it in its unfermented form.
Myth #4: Soy is a phytoestrogen.
Fact: The term phytoestrogen describes the ability of certain compounds (found in foods and medicinal herbs) to act similarly to the actions of the hormone oestrogen. However, incorrect interpretations of the term phytoestrogen have raised some concern.
As it pertains to soy, experts have corrected the term phytoestrogen, defining the bean instead as a selective oestrogen receptor modulator or ‘SERM’.
Being a SERM, soy communicates with the body similarly to oestrogen as it can bind to what’s known as oestrogen ‘receptors’, which then modulates their activity (the ‘output’). For example, soy isoflavones have been shown to down-regulate oestrogen receptor alpha (ER-α) activity. Given that ER-α is associated with negative events such as tumour growth, SERM compounds (like the isoflavones found in soy) are viewed as beneficial, as they can favourably influence the state of play. What’s more, soy isoflavones also bind to the beneficial oestrogen receptor beta (ER- β), whose activity is associated with protective health benefits in both men and women.9 In summary, a SERM such as soy does not increase oestrogen levels, but balances oestrogen receptor activity, which can lead to more optimal body function.
The Balance of Soy
It’s important to keep in mind that the health benefits of soy, like many wholefoods, are broad. The soybean is much more than just soy isoflavones – it provides additional health-promoting nutrients including protein, fibre, minerals and B vitamins, all nourishing your body in more ways than one. To enjoy some soy as part of a balanced, check out the healthy Tofu and Veggie Stir-Fry recipe below. You too can reap the benefits of this highly versatile legume.
Tofu and Veggie Stir-Fry

Makes 1 serve.
Ingredients:
• 1 tablespoon of olive oil
• 200 g tofu
• 50 g broccoli
• 50 g cauliflower
• 1 clove garlic (cut into small pieces)
• 1 tablespoon of diced chives
• 1/3 cup water
Method:
• Heat oil with garlic until garlic is lightly cooked.
• Add cauliflower, tofu and broccoli and stir through very quickly.
• Add water and continue stirring.
• Cook on high heat for approximately four minutes and continue stirring.
• Add a little more water if required to prevent sticking.
• Add chives.
• Turn out and serve.
References
1. Messina M, Redmond G. Effects of soy protein and soybean isoflavones on thyroid function in healthy adults and hypothyroid patients: A review of the relevant literature. Thyroid. 2006 Mar;16(3):249-258. doi: 10.1089/thy.2006.16.249.
2. Soukup ST, Helppi J, Müller DR, Zierau O, Watzl B, Vollmer G, et al. Phase II metabolism of the soy isoflavones genistein and daidzein in humans, rats and mice: a cross-species and sex comparison. Arch Toxicol. 2016 Jun;90(6):1335-1347. doi: 10.1007/s00204-016-1663-5.
3. Messina M. Soy and health update: evaluation of the clinical and epidemiologic literature. Nutrients. 2016 Nov;8(12):1-42. Doi: 10.3390/nu8120754.
4. Messina M, Redmond G. Effects of soy protein and soybean isoflavones on thyroid function in healthy adults and hypothyroid patients: A review of the relevant literature. Thyroid. 2006 Mar;16(3):249-258. doi: 10.1089/thy.2006.16.249.
5. EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS). Risk assessment for peri‐and post‐menopausal women taking food supplements containing isolated isoflavones. EFSA Journal. 2015 Oct;13(10):4246. doi: 10.2903/j.efsa.2015.4246.
6. Rizzo G, Baroni L. Soy, soy foods and their role in vegetarian diets. Nutrients. 2018 Jan 5;10(1):43. doi:10.3390/nu10010043.
7 EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS). Risk assessment for peri‐and post‐menopausal women taking food supplements containing isolated isoflavones. EFSA Journal. 2015 Oct;13(10):4246. doi: 10.2903/j.efsa.2015.4246.
8. Rizzo G, Baroni L. Soy, soy foods and their role in vegetarian diets. Nutrients. 2018 Jan 5;10(1):43. doi:10.3390/nu10010043.
9. Kuiper GG, Lemmen JG, Carlsson B, Corton JC, Safe SH, van der Saag PT, et al. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology. 1998 Oct;139(10):4252-4263.
Get to do this for patients every day!💞
Check Out the latest WELLNESS REVIEW!👀🍃

It’s a great weekend to… 🧘♀️🌄🙏