Less ideal is how feeling under pressure or stressed decreases digestive function – this is because when your body-mind perceives ‘danger’ (which is what stress is from a physiological sense – see this article here), then it’s not a priority to be eating, therefore digestion suffers and you may experience bloating or heartburn or some other uncomfortable symptom.
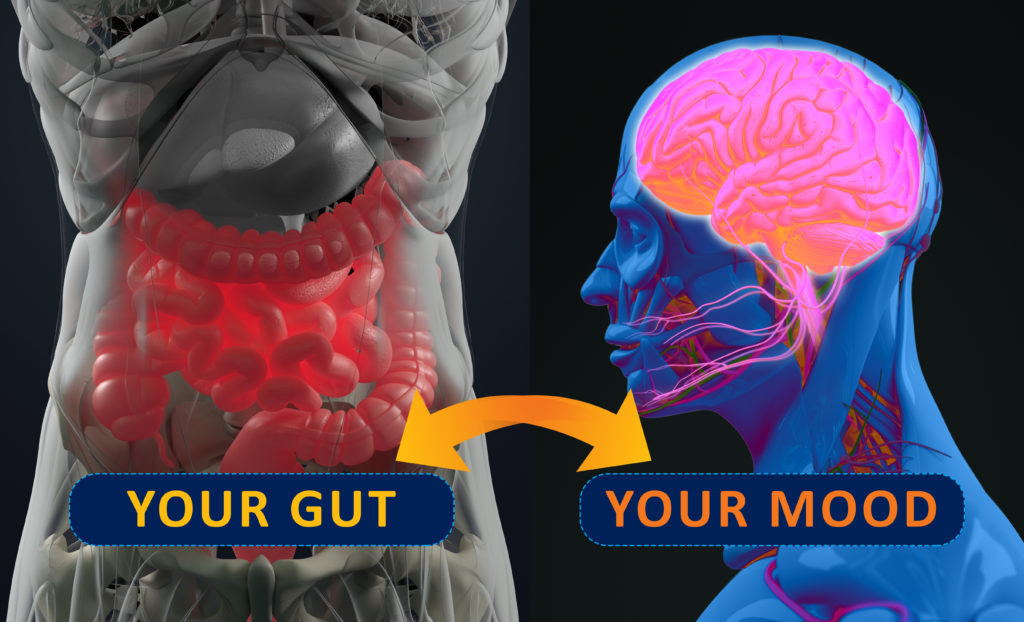
Knowing this mind-gut link exists can help explain how feeling anxious may impact how your gut is functioning, but perhaps more significant (though not as well known) is that what’s going on in your gut could also be impacting your mental health.
Lighting a Fire in the Brain
Though the causes may be multifactorial, a key player in this situation is gut-derived inflammation. This can result from dysbiosis, which is an imbalance in your gut microbiota (the microbial life that resides within your intestines), and/or some degree of insult to the digestive tract lining – your gut ‘barrier’. Both your gut barrier and your microbiota work synergistically to support effective digestion, immune health, and overall wellbeing. However, if they become disrupted then biochemical signals or ‘cytokines’ are released that travel throughout your body causing what’s referred to as oxidative stress in any number of tissues in your body including your brain.
Though many of these cytokines cannot cross what’s called the blood-brain-barrier, their presence triggers similar ‘alarm’ signals in the brain so it too is impacted by its own inflammatory processes. This sequence of events can be why symptoms such as poor mood, brain fog and anxiety occur; but for those who want a more specific example – inflammation can promote the neurotransmitter precursor tryptophan to produce quinolinic acid[1] instead of serotonin and melatonin – the former situation leading to what can most simply be described as nerve cell ‘agitation’ that can present as anxiety.[2]
Soothe Your gut to Settle Your Mind
As gut health is fundamental to all aspects of wellbeing then any symptoms really need to be attended to – and to do that with the least guesswork then my recommendation is to see a natural healthcare Practitioner who can help you navigate what may be the contributing causes for you, e.g. do you need to tweak your diet? Get some help with digesting certain foods? Heal your gut barrier? Equally, if you are struggling with stress, sleep, or experiencing regular mood problems then speak to your Practitioner about this too – there are many natural medicine solutions available, but to find the best ones for you will require assessing your personal situation first.

Is it too Early to Rely on Psychobiotics?
If you are already a fan of natural medicine you may be wondering what the role of probiotics are in this, particularly as there is emerging talk of ‘psychobiotics’ or probiotics that can impact mood. This is clearly of interest to those who may be experiencing stress or anxiety, so I’d say to you that the human evidence for what may be the ‘best’ probiotic strain and at what dose to help is still in its infancy; but watch this space for future research developments.
What we do know currently is that supporting whole gut health by decreasing gut-derived inflammation and increasing the diversity of the gut microbiota is a proven clinical approach to whole-body wellbeing – and this includes improving mental health.
So if you experience symptoms impacting either your mind or your gut, please don’t put up with them any longer, or try to figure it all out on your own. Contact your Clinical Naturopath or Integrative Doctor and let them know what’s going on, so they can personalise a solution for your situation.

[1] Lugo-Huitrón R, Muñiz PU, Pineda B, Pedreaza-Chaverri J, Rios C, Pérez-de la Cruz V. Quinolinic acid: an edogenous neurotoxin with multiple targets. Oxidative Medicine and Cellular Longevity. 2013;Article ID 104024, 14 pages. Available from: https://www.hindawi.com/journals/omcl/2013/104024/
[2] Bryleva EY, Brundin L. Kynurenine pathway metabolites and suicidality. Neuropharmacology. 2017 Jan;112(Pt B):324-330. doi: 10.1016/j.neuropharm.2016.01.034. Epub 2016 Jan 26. Available from: https://www.sciencedirect.com/science/article/pii/S0028390816300338

